Direct Financing of Health Facilities. Experiences from financing reforms in Tanzania.
1.1 Background and study objectives
1.4 Study areas and implementation timelines
1.5.2 Data sources and sampling
2.1 Research questions and key findings
2.3.3 Implementation of e-systems (PlanRep and FFARS)
3. Obtaining and spending funds
3.1 Research questions and key findings
3.2 Understanding of how RBF and HBF-DHFF funds are obtained
3.3 How are RBF and HBF-DHFF funds budgeted and spent?
3.3.1 How budgeting and spending decision are made
3.3.2 What the funds are spent on
4. Effects on service delivery and governance
4.1 Research questions and key findings
4.2 Effects on the organisation and delivery of services
4.2.3 Perceptions of the impact of RBF and HBF-DHFF
4.3 Factors that facilitated or inhibited change in service delivery
4.3.1 RBF design and RBF effects
4.4 Effects on governance and accountability
4.4.1 Effects on Health Facility Governing Committees (HFGCs)
4.4.2 Effects on the relationships between district managers and health facilities
5. Effects of RBF on community health worker performance
5.1 Research questions and key findings
5.2 Community health worker performance
5.3 Factors that facilitated or inhibited change
6. Effects of RBF on nutrition-related interventions
6.1 Research questions and key findings
6.3 Nutrition services at health facilities
6.4 Nutrition services through community health workers
6.5 Factors that facilitated or inhibited change
How to cite this publication:
Ottar Mæstad, Jo Borghi, Farida Hassan, Eskindir Shumbullo Loha, John Maiba, Iddy Mayumana, Vincent Somville, Sarah Tobin, Peter Binyaruka (2021). Direct Financing of Health Facilities. Experiences from financing reforms in Tanzania.. Bergen: Chr. Michelsen Institute (CMI Report 2021:10)
CMI Brief 2021:5: Towards harmonised financing of frontline health service providers in Tanzania.
CMI Report 2021:07: Results-based financing in the health sector in Tanzania. Process evaluation. Phone Survey #1.
CMI Report 2021:08: Results-based financing in the health sector in Tanzania. Process evaluation. Phone Survey #2.
CMI Report 2021:09: Direct health facility financing in Tanzania. Process evaluation. Phone Survey #3.
Executive summary
This study aims to understand how mechanisms for direct financing of health facilities in Tanzania have worked, and what factors have facilitated or inhibited their success.
We consider two new financing mechanisms: Results Based Financing (RBF), implemented in selected regions from 2015 onwards, and Direct Health Facility Financing of Health Basket Funds (HBF-DHFF), implemented nationwide from the financial year 2017/18.
Objectives of direct facility financing: Both financing mechanisms aim to improve the quality of health services, improve efficiency, and to mobilise human resources at facility and community levels for improved health services. In the case of RBF, it is also a clearly stated objective to increase service utilisation.
Key characteristics of RBF and HBF-DHFF: Both schemes enhance the autonomy of primary health care facilities in planning, budgeting and managing resources, and both involve elements of output-based financing. Among the differences are that RBF has a more comprehensive set of performance indicators and incentive mechanisms, including incentives for health workers and community health workers. RBF also involves fewer restrictions on how resources can be spent.
The study is based on data from the Mwanza and Mara regions from the period 2016 to 2020. We utilise the fact that Mwanza implemented RBF three years earlier than Mara to study what difference RBF made.
Both financing mechanisms were largely implemented as planned. However, there was a substantial delay in RBF payments from the end of 2018 onwards due to additional reporting requirements from the Ministry of Finance and Planning. Training was also implemented as planned, but there is room for improvement in training in HBF-DHFF, as inadequate training was reported by a substantial share of facility in-charges. Most in-charges were uncertain about payment criteria for HBF-DHFF. There is also potential for making more and better use of the digital planning and budgeting tool (PlanRep).
There is large variation in how RBF performance verification has been experienced by facility staff. Some report that verification has worked very well, while others point to challenges in the interaction with facility staff. It is commonly reported that unintentional and accidental errors continue to be penalised.
RBF had a significantly positive impact on reported service utilisation. We identified a positive change in eight out of twelve incentivised services. There is a particularly consistent pattern of increased utilisation of maternal health services, both antenatal care, institutional deliveries, and post-natal care. It took between one and two years before the increase started to materialise.
The data is also consistent with a positive effect of HBF-DHFF on service utilisation, especially maternal health services. After the implementation of HBF-DHFF, there was a significant increase in the use of maternal health services in both regions. We do not have direct evidence of a causal link between HBF-DHFF and this increase, but HBF-DHFF seems to have initiated some of the same positive effects on service quality as RBF, especially improved drug supply.
Facility in-charges claim that the main features of RBF contributing to the positive change are 1) additional funding, 2) incentives for facilities and health workers, 3) performance monitoring and verification visits, and 4) increased autonomy and control over funds and their use. These features were claimed to improve the morale of health workers and their ability to do their job, make health workers more ‘client orientated’, reduce absenteeism, improve team work, make supervision more results focused, and make more facilities boost the demand for health services. Facility in-charges also claimed that drug supply improved significantly.
The main feature associated with positive effects of HBF-DHFF is increased autonomy, which reduced the need to pass through bureaucratic processes to access funds. This enabled facilities to utilise resources more efficiently, and to improve drug supply in particular. The perceived impact of HBF-DHFF on the availability of drugs and supplies was however not as strong as the impact of RBF. Even though HBF-DHFF gradually has included stronger elements of output-based financing, these incentives were not emphasised as important contributors to change in the case of HBF-DHFF.
RBF, to a greater extent than HBF-DHFF, seems to have spurred a problem-solving attitude at health facilities. While budgeting and spending decisions with RBF have been ‘bottom-up’ and ‘needs-based’, HBF-DHFF budgeting and spending decisions have to a larger extent been ‘top-down’ and ‘rules-based’.
Restrictions on how HBF-DHFF funds can be budgeted and spent were seen as a major constraint by a majority of facility in-charges, while regulations on how to use RBF funds were to a much lesser extent seen to restrict the facilities’ ability to improve service delivery.
The delay in RBF payments from end of 2018 does not seem to have seriously impacted service utilisation. This may appear somewhat puzzling in light of the importance attributed to additional resources in improving service delivery. One potential explanation is that service demand is sticky: although the quality of services may have declined somewhat, it takes time to reduce service demand, just as it took time for RBF to increase service utilisation in the first place. Moreover, the implementation of HBF-DHFF may have contributed to maintain the quality of services through its positive effect on drug supply. Finally, most health workers continued to believe that they would eventually receive their bonuses, which implies that the incentive mechanisms were still in effect even though payments were delayed.
Both RBF and HBF-DHFF have strengthened governance mechanisms at the community level. There have been more frequent meetings in Health Facility Governing Committees and greater involvement of these committees in budgeting and spending decisions. Both RBF and HBF-DHFF increased the committees’ ‘voice’ and influence on facility functioning.
RBF and HBF-DHFF have also created new forms of mutual dependency between facilities and the district level. Greater transparency around the allocation of basket funds has improved providers’ attitudes towards district managers and reduced conflict within the district. However, some district managers were unhappy about their loss of power.
RBF created a mutual dependency between health facilities and community health workers which improved their cooperation and trust and facilitated higher utilisation of health services. This was facilitated by the incentives provided to community health workers for escorting women for delivery and for doing home visits. Community health workers report that RBF has significantly increased the number of women escorted for delivery. Many community health workers also report that RBF increased the number of household visits. However, on average CHWs did not report a higher number of household visits in 2020 than they did in 2016.
This study also looked specifically at the potential impact of RBF on nutrition-related services. RBF may have contributed towards the significant reduction in stunting that took place in Mwanza between 2014 and 2018, along with several other interventions that focused specifically on nutrition.
A large share of facility in-charges in Mwanza claim that RBF has a significant impact on nutrition services, especially through more consistent provision of nutritional supplements and drugs. RBF is perceived to reduce stock outs of nutritional supplements and drugs, both because of the additional resources and the incentives. Very few facilities in Mwanza had a stock out of nutrition-related drugs and equipment during our 2020 visit. While RBF may have contributed to this change, other factors have likely contributed, too.
Community health workers also seem to play an important role for improved nutrition. RBF is claimed to have made community health workers bring more women and children to health facilities to receive nutrition services, especially through early antenatal care visits. Most community health workers can provide relevant and valuable nutrition-counselling services. However, we do not know for sure whether RBF led community health workers to provide nutrition counselling to more women. Although there are several indications that it did, some data point in the opposite direction.
A more comprehensive summary of findings is presented at the beginning of each chapter.
1. Introduction
1.1 Background and study objectives
Many low-income countries are implementing health financing reforms to achieve universal health coverage (Kutzin 2013; WHO 2010). For instance, various forms of performance-based financing are implemented in many developing countries (Meessen et al. 2011; Renmans et al. 2016). In Tanzania, a pay-for-performance (P4P) scheme was piloted in the Pwani region in 2011–2014 (Binyaruka et al. 2015; MoHSW 2012), and a different performance-based program was rolled later on out to other regions under the label Results-based Financing (RBF) (MoHSW 2015). RBF was phased in gradually from 2015 and is currently being implemented in nine regions.
Since 2017, Tanzania has also provided direct financing of health facilities through direct transfer of heath sector basket funds from the central government to health facilities’ bank accounts (Kapologwe et al. 2019; MoHCDGEC 2017). This mechanism, the HBF-DHFF, has been implemented in primary health care facilities in all regions in Tanzania.
Although both RBF and HBF-DHFF are mechanisms for transferring funds directly to health facilities, there are several differences between the schemes, possibly implying different impacts on the health system. The motivation behind this study is to learn from experiences with the two systems to date, in order to further improve the mechanisms for health financing in Tanzania.
Moreover, there has been a particular interest among stakeholders in looking at how RBF may have affected nutrition-related health services.
The study thus has two main objectives:
- To understand how the RBF and HBF-DHFF financing mechanisms have worked and factors that inhibit or facilitate their success.
- To assess how RBF has affected the delivery of nutrition-related interventions at the health facility and community levels.
1.2 RBF and HBF-DHFF in brief
RBF and HBF-DHFF emerged out of quite different processes, but the two systems have gradually become more closely aligned. RBF was a new financing mechanism and a new source of donor funding which came on top of already existing funding sources. RBF was implemented with a strong focus on improving the performance of health facilities and came (at least partially) with its own systems of performance monitoring, verification, planning, and accounting. The planning and accounting systems have later been aligned with those of HBF-DHFF.
HBF-DHFF is a new way of allocating and managing the Health Basket Funds, provided by a group of development partners. HBF-DHFF can be seen as one further step in ongoing processes of Decentralization-by-Devolution in Tanzania, in this case the devolution of planning and financial management to the primary health care level. By gradually putting more weight on facility performance in its allocation formula, HBF-DHFF has become more similar to RBF over time.
1.2.1 Objectives
The objectives of RBF and HBF-DHFF are almost identical. Both schemes aim to improve the quality of health services, improve efficiency, and to mobilise human resources at facility and community levels for improved health services. The background documents suggest however that RBF, at least initially, had a stronger emphasis on increasing service utilisation. HBF-DHFF, on the other hand, had an explicit focus on reducing the inefficiencies resulting from wasted time and delays in the existing system (MoHCDGE and PROALG, 2017). The detailed objectives are summarised below. A further description of the underlying theories of change is provided in Appendix 1.
RBF objectives: The main goal of RBF is to improve the utilisation and quality of services offered to the community (MoHSW, 2015). The specific goals are to:
- Improve the accessibility and utilisation of health care services
- Improve the quality of health services at all facilities
- Improve the productivity and efficiency of service delivery by health care providers
- Improve the quality and use of data for evidence-based decision making
- Improve accountability and responsiveness of health management teams and facility governing committees
- Provide equitable access to cost-effective quality health care.
HBF-DHFF objectives: The objectives of HBF-DHFF are (GoT, 2017):
- To Improve quality of services
- To further decentralise health services management (deepening Decentralization-by-Devolution)
- To Improve efficiency and effectiveness of resources use and management, transparency and autonomy
- To enhance community empowerment and ownership of health services; mobilisation of resources and planning.
1.2.2 Key characteristics
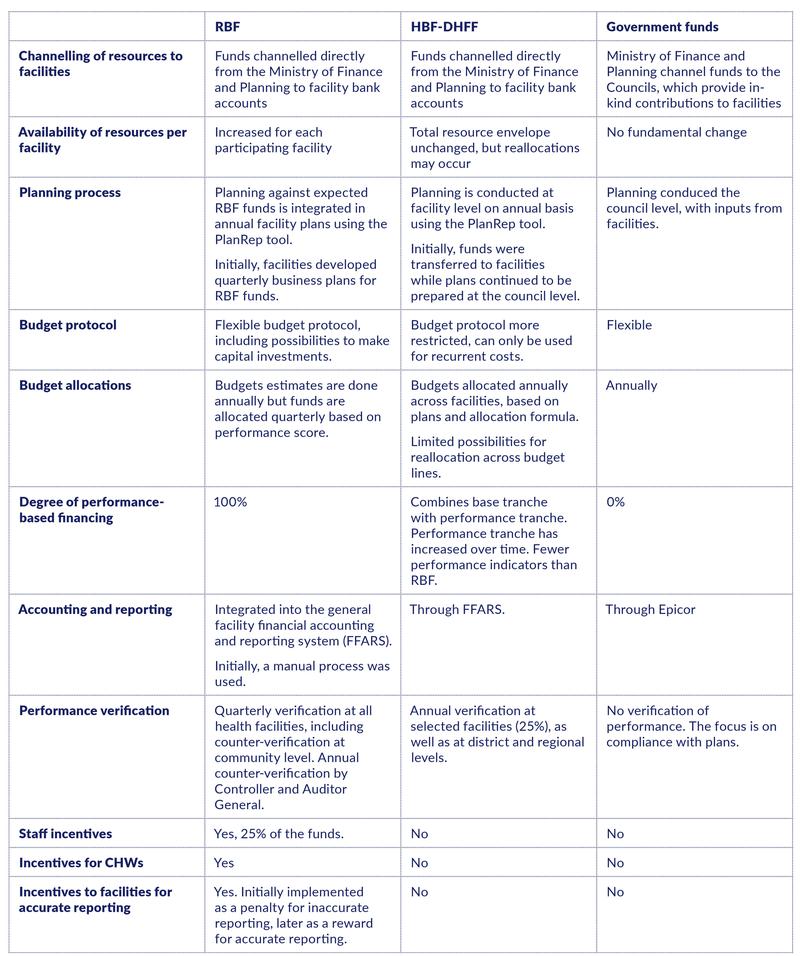
Key characteristics of RBF and HBF-DHFF are summarised in Table 1. For comparison, a separate column for government funds is also included.
RBF and HBF-DHFF are similar in the following respects:
- Health facilities receive financial resources directly from the Ministry of Finance and Planning to the facilities’ bank accounts.
- Planning is conducted annually using the PlanRep tool.
- Health Facility Governing Committees are supposed to be directly involved in planning processes.
- Accounting and reporting are done through the FFARS system.
- Include output-based financing mechanisms.
RBF and HBF-DHFF differ in the following respects.
- RBF increases total resources available to the facilities, while HBF-DHFF replaces previous in-kind transfers.
- RBF has a more flexible budget protocol, with possibilities to also budget for capital investments.
- RBF funding is solely based on performance, while HBF-DHFF includes a base tranche allocated based on catchment population and distance to the headquarters of local government authorities.
- RBF includes a larger set of performance indicators with 16 indicators on service utilisation and 18 groups of indicators on service quality. HBF-DHFF includes four indicators on service utilisation and two indicators on service quality.
- RBF involves performance reporting and payments every quarter, while HBF-DHFF is based on annual figures.
- RBF involves more comprehensive verification of performance scores at health facility and community levels.
- RBF includes bonus payments for health workers (25% of the funds) while all HBF-DHFF funds go to facility operations.
- RBF includes incentives to community health workers for conducting household visits, escorting women to health facilities for delivery, and reporting maternal and perinatal deaths.
- RBF includes incentives for accurate reporting.
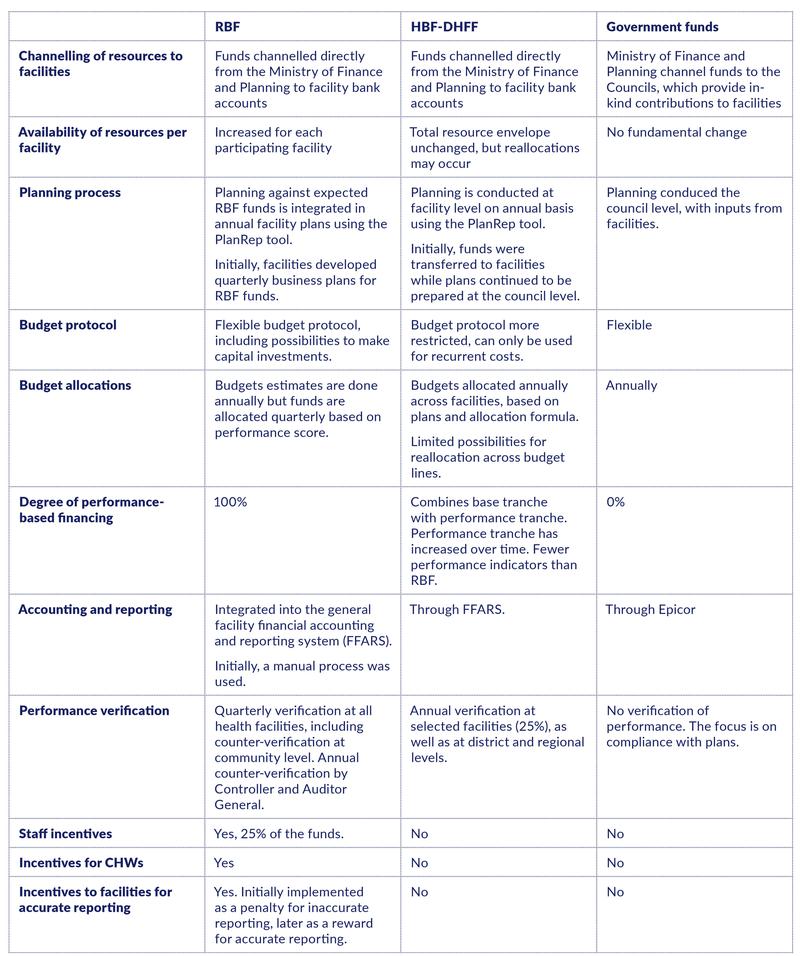
Table 1.1. Characteristics of RBF and HBF-DHFF.
1.3 Main research questions
Objective 1: Understand how the RBF and HBF-DHFF financing mechanisms have worked and factors that inhibit or facilitate their success.
- To which extent have RBF and HBF-DHFF been implemented as planned? What are the reasons for any deviations?
- What are facilities’ understanding of how RBF and HBF-DHFF funds are obtained?
- How have funds been flowing to the facilities through RBF and HBF-DHFF?
- How are RBF and HBF-DHFF funds spent and how are decisions about spending made? What is prioritised for spending, and why?
- How have RBF and HBF-DHFF affected the organisation and delivery of services?
- Which aspects of the schemes and which contextual factors have facilitated or inhibited change?
- How have RBF and HBF-DHFF affected governance and accountability mechanisms, including tools and processes at health facilities and the relationship between different levels of the health system?
- How has RBF affected the performance of CHWs?
Objective 2: Assess how RBF has affected nutrition-related interventions at the health facility and community level.
- This objective involves an in-depth investigation of one particular area in which RBF is intended to affect service delivery. The overarching research questions are:
- How has RBF affected the provision of nutrition services at health facilities?
- How has RBF affected the provision of nutrition services by CHWs?
- Which factors have facilitated or inhibited change?
- How has RBF affected the relationship between CHWs and the facility?
- To which extent have other donor-financed programmes contributed to improved nutrition services? How?
1.4 Study areas and implementation timelines
This study was conducted in public health facilities in the Mwanza and Mara regions. All districts in the two regions were included, covering a mix of rural, urban, and peri-urban areas.
The main rationale for the choice of study areas is that RBF was implemented at different points in time in the two regions. While RBF started in Mwanza in 2016, it did not start until 2019 in Mara. This allows for studying the impact of RBF in Mwanza by using Mara as a control region.
HBF-DHFF was implemented in both regions at the same time, effectively starting during the first quarter of 2018 (see Figure 1.1).
Implementation of RBF in Mwanza started in the second quarter of 2016. Training of health workers started in April, while district level managers were trained a few months later. Collection of performance data also started in the second quarter, while the first RBF payments were made during the fall of 2016. Quite a few health facilities were not eligible for RBF from the start, implying that implementation was more gradual than the figure suggests.
Implementation of RBF in Mara started in the third quarter of 2019. Training was conducted in July. While RBF performance data have been collected from the start, RBF payments had yet not been receied in Mara when data collection for this study was conducted in March 2020.
Another difference between the two regions is that facilities in Mwanza received a start-up grant of 10 mill TSH when RBF started, while no such grant was provided in Mara.
The implementation of HBF-DHFF started nationwide during February 2018 (Kapologwe et al., 2019).
1.5 Methods and data
1.5.1 Study design
We used a mixed-method study design with both qualitative and quantitative methods.
Qualitative interviews were conducted with community health workers, health facility in-charges, and health managers at district, regional, and national levels during the first quarter of 2020.
Quantitative data were collected through surveys at health facilities, with health workers, and with community health workers, also during the first quarter of 2020.
A baseline survey was conducted in both regions during the first quarter of 2016. This allows for before-after analysis, as well as analysis of the impact of RBF by comparing changes across regions over time.
1.5.2 Data sources and sampling
Quantitative data
The sampling frame included all public health facilities at dispensary and health centre levels. Facilities were stratified according to their star rating (i.e., the government’s assessment of structural quality) at baseline. We selected a proportionate random sample of health facilities within each stratum, a total of 75 facilities in each region. At each facility, we surveyed up to two randomly selected health workers and up to two randomly selected community health workers.
The final sample includes 150 health facilities, 294 health workers, and 294 community health workers. The same health facilities were included at both baseline and endline, while some health workers are not necessarily the same.
Qualitative data
The sampling frame was the list of 150 facilities included in the quantitative survey. In each district, we randomly selected around 1/3 of these facilities for qualitative data collection. Facilities were stratified into high and low baseline performance strata, using the star ratings assigned by the government, and were then selected using proportionate random sampling.
Fifty facilities were sampled in total, 25 in each region. In both Mara and Mwanza, we sampled 11 facilities with a star-rating of 0 and 14 facilities with a star-rating of 1 or 2. At each facility, we conducted one qualitative interview with the facility in-charge and one interview with a community health worker (one of whom were also included in the quantitative survey).
The final sample included 48 interviews with health facility in-charges and 44 interviews with community health workers.
At district and regional levels, 16 respondents were purposely selected for qualitative interviews. Respondents include stakeholders who had been involved in RBF/ HBF-DHFF implementation and/or had an overall responsibility for service delivery (e.g., District Medical Officers or RBF coordinators). We also conducted two qualitative interviews with national level stakeholders at ministry level.
Thus, the qualitative data consists of 110 interviews in total.
Secondary data
We used routine administrative data from DHIS2 on service utilisation to assess performance over time. We also utilised RBF process evaluation data collected through two rounds of phone surveys with health workers and community health workers at the 75 facilities in the Mwanza region where we already collected baseline data. Finally, we drew on qualitative process monitoring data from four rounds of data collection between 2016 and 2018, including interviews with health workers, community health workers, managers, and members of health facility governing committees in three districts in Mwanza region.
1.5.3 Data analysis
Qualitative data analysis
Qualitative data were transcribed and translated from Swahili to English. Interviews were analysed theme by theme, and responses were systematised and compared across regions and across facilities with different star-ratings at baseline. Results were compared with and analysed in relation to findings from the quantitative surveys.
Analysing impacts of RBF using administrative data
We analysed the impact of RBF by comparing changes over time in service utilisation data in Mwanza and Mara (i.e., difference-in-difference analysis). We estimated impacts on each of the incentivised service utilisation indicators independently. Service utilisation data was from DHIS2, i.e., before RBF verification. One reason for not using the verified data is that verification was conducted in Mwanza only, implying that the verification process itself would be a potential source of bias. Another reason is that the DHIS2 data include data from before the implementation of RBF, which allows for testing of whether the performance evolved along parallel trends before RBF implementation. If trends were parallel, our estimates of impacts will be more credible.
We measured the effect of RBF by comparing performance in Mwanza and Mara from the beginning of the second quarter in 2016 (when RBF started in Mwanza) until the end of the second quarter in 2019 (when RBF started in Mara), utilising data from each quarter throughout this period. This results in a conservative estimate of the effects of RBF for the following reasons: (1) not all facilities in Mwanza were included in the RBF scheme from the start; (2) it takes time for an intervention like RBF to take effect, and our measure does not account for this; and (3) insofar as RBF payments in themselves contribute to impacts, our measure will provide an underestimate since RBF payments were not received in all quarters throughout this period (see more about delays in payments in Chapter 2).
Since HBF-DHFF was implemented in both regions at the same time, this reform does not necessarily have any impact on our estimates of the impact of RBF. However, it is also conceivable that HBF-DHFF biases the estimates of the impact of RBF upwards (if HBF-DHFF boosts the effect of RBF in Mwanza) or downwards (if HBF-DHFF makes more of a difference in Mara where facilities had less direct financing at the outset). To shed further light on this issue, we measured the impact of RBF also for the period up to the implementation of HBF-DHFF only, until the first quarter of 2018.
All estimates of the impact of RBF are calculated by controlling for confounding variables at the facility level through facility-level fixed effects. Standard errors are clustered at the facility level.
Analysing impacts of RBF impacts using other quantitative data
Other quantitative data used to analyse changes over time are available only at baseline (first quarter of 2016) and endline (first quarter of 2020). Since endline took place after the implementation of RBF in Mara, these data cannot straightforwardly be used to analyse the impacts of RBF. On the other hand, since the implementation time in Mara had been short and it takes time for the intervention to take effect, the bias is not necessarily huge. If there is a bias, effect sizes are likely to be underestimated.
Note here as well that the implementation of HBF-DHFF may (or may not) complicate the interpretation of results. It is therefore important to treat results about impacts based on these data with care.
1.6 Ethics
Ethical clearance was obtained from national and institutional ethics committees in Tanzania. The institutional ethical approval is from the Ifakara Health Institute, while the national approval is from the National Institute of Medical Research (NIMR).
We sought written informed consent from all respondents by providing information on the objectives of the research and the procedures applied in a clear language using an information sheet.
2. Implementation issues
2.1 Research questions and key findings
This chapter addresses the following research questions:
- To which extent have RBF and HBF-DHFF been implemented as planned? And what are the reasons for any deviations?
Key findings on RBF implementation include:
- RBF training was conducted as planned and was adequately received in both regions. However, there seems to be a need for refresher training for new staff, especially in Mwanza.
- In-charges report that RBF data verification was largely implemented as planned, despite significant delays. Counter-verification by tracing patients at the community level was conducted in most places, but almost a fifth of the facilities reported that this did not happen at all.
- There is large variation in how verification has been experienced by facility staff. Some report that verification has worked very well, while others point at challenges in the interaction with facility staff.
- It is commonly reported that unintentional and accidental errors continue to be penalised.
- Delayed payment was the main implementation challenge in both regions. Payments have been delayed for more than a year in Mwanza.
- Payment delays were mainly caused by additional reporting requests from the Ministry of Finance and Planning.
- Almost all health workers claimed that services provision continued as normal despite delays in RBF payments. However, some planned activities could not be performed, and some community health workers were clearly demotivated. Delays in payments also caused delays in subsequent verification.
- Most health workers believed that payments would eventually arrive. This may have reduced the negative impacts on service delivery.
Key findings on HBF-DHFF implementation include:
- HBF-DHFF training was implemented as planned. However, a substantial share of facility in-charges found the training inadequate. Short training time and a lack of computer skills were key obstacles to receiving adequate training.
- HBF-DHFF payments were largely made as planned, except for delayed disbursements for the last two quarters of 2019. Delayed HBF-DHFF disbursements were reported to reduce service quality.
- E-systems (FFARS and PlanRep) were largely implemented as planned, but some remote areas lack the power supply and internet required for their operation.
- Deployment of facility accountants was seen as a crucial decision, but some dispensaries received inadequate support, perhaps due to limited financial resources to support visits by the accountants.
- There is room for improvement in making active use of PlanRep in planning and budgeting.
2.2 RBF implementation
2.2.1 RBF training
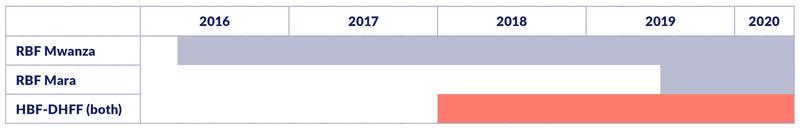
RBF training was conducted as planned and was adequately received in both regions. However, there seems to be a need for refresher training for new staff, especially in Mwanza. The introduction of RBF involved training of health workers, community health workers (CHWs), representatives of health facility governing committees (HFGCs), and health managers. Training was successfully conducted in April 2016 in the Mwanza region and in July 2019 in the Mara region. Representatives from each facility attended the training session and provided feedback to their colleagues who did not attend. In the health facility survey, we found that most in-charges confirmed that they had received adequate training “to a high extent”. Only 12% (in Mwanza) and 7% (in Mara) responded “to a low extent” (Figure 2.1). More recent training in Mara than in Mwanza might explain the slightly higher satisfaction with the training in Mara. Some of the in-charges and managers in Mwanza recommended a refresher training since some staff were newly recruited or transferred and therefore have inadequate knowledge about RBF.
2.2.2 RBF data verification
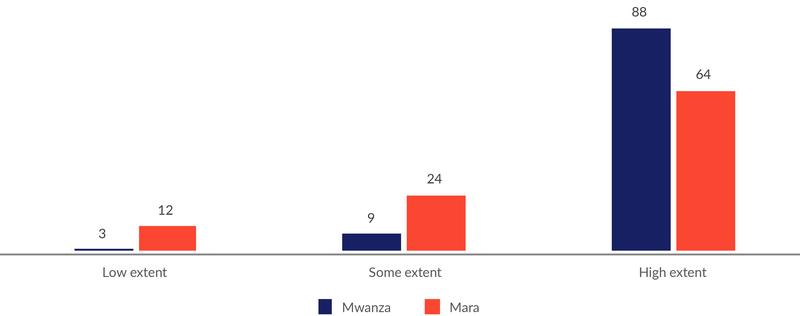
In-charges report that RBF data verification was largely implemented as planned, despite significant delays. Most in-charges claimed that data verification was implemented as planned “to a high extent” (i.e., 88% of in-charges in Mwanza, and 64% in Mara).
These figures are somewhat surprising considering the challenges with delayed verification: The verification implemented in January-March 2020 covered not only the previous quarter, but all quarters back to October-December 2018 (except April-June 2019, which had been verified in July 2019). In Mara, this was the first verification since RBF started in the third quarter of 2019. These delays frustrated some facility in-charges, especially those who had prepared well. One in-charge said,
“A delay in conducting verification in time demoralised people. Yes, some people started to think that (…) they might not come the way we were told, and to the extent of some people saying possibly RBF is no longer existing.”
Counter-verification by tracing patients at the community level was conducted in most places, but almost a fifth of the facilities reported that this did not happen at all. In a phone survey in 2018, 78% of health workers in Mwanza stated that patients were traced in communities, and among those who confirmed this, 89% reported that it had happened recently (i.e., in 2018). 18% said that tracing patients was not done at all.
There is large variation in how verification has been experienced by facility staff. Some report that verification has worked very well, while others point at challenges in the interaction with facility staff. Some said that verification was conducted in a friendly atmosphere by well-trained verifiers. According to one in-charge:
“When the verifiers come, they are not harsh, they are friendly and they work in a friendly way, when they come and find that you are busy, they wait for you to first provide services to the clients.”
Others reported that verifiers were often in a rush, poorly engaging with local facility staff.
“We couldn’t have time to sit with verifiers. They just proceeded with verification alone as we continued delivering health services to many patients awaiting services. So, whatever we were supposed to clarify to them, we were not given that opportunity to do that. As a result, the marks we were awarded were unrealistic”. (Facility in-charge, Butiama district council, Mara)
Some verification teams lacked sufficient medical competence or had insufficient understanding of the health system, which led to incorrect scores.
“They were all not from the medical field, hence an individual would come to verify things which he/she does not understand, something which brought a lot of challenges and sometimes rose unnecessary arguments. They even led to other facilities not getting their rights because the individual doing the verification does not understand”. (Facility in-charge, Kwimba district council, Mwanza)
Some verifiers, especially in Mwanza, provided contradictory instructions about how particular indicators are measured, giving different instructions at different rounds of verification.
It is commonly reported that unintentional and accidental errors continue to be penalised. This was reported by nearly all respondents and at all levels. This is a puzzling finding in light of the fact the RBF system changed already in 2017 from a carrot-stick approach, with penalties for reporting errors, to a carrot-carrot system, with rewards for correct reporting. But it is in line with findings from our November 2018 phone survey, where almost 90% of health workers still believed that the carrot-stick approach was in force.
2.2.3 RBF payments
Delayed payment was the main implementation challenge in both regions. Payments have been delayed for more than a year in Mwanza. RBF payments are supposed to be made after each quarters’ verification. In Mwanza, this was initially implemented as planned. However, towards the end of 2018, after the July-September verification, but before RBF payments had been made, it was decided to stop further payments. No further payments were made to facilities until early 2020, when they received for July-September 2018. Hence, at the time of our data collection, payments had been made neither for the last quarter of 2018 nor for the whole of 2019. No facility in Mara had received any RBF payments at the time of our study, implying a delay of around three months.
Delays in payments were mainly caused by additional reporting requests from the Ministry of Finance and Planning. The Ministry requested to assess RBF spending since inception, which required expenditure reports for each facility.
“The Ministry of Finance and Planning restricted disbursement of all RBF money to facilitators [PORALG] and health facilities, until they are done with the auditing of costs and expenditures of all health facilities implementing RBF. The process took almost eight months, because facilitators were not aware of the process so they could not have all the documents at hand”. (National stakeholder at the Ministry level)
Delays in payments caused delays in subsequent verification. No further verification of performance took place while past RBF expenditures were being assessed. When verification resumed in July 2019, only (April-June 2019) was verified, leaving performance data for Oct-Dec 2018 and January-March 2019 unverified. Performance data for these quarters were not verified until February 2020.
According to our informants, these delays were caused by lack of funding for conducting verifications, as such funding is released with reimbursements for RBF payments made for previous periods. However, if such funding has been lacking, it is unclear why verification nevertheless was done for April-June 2019. It is also unclear why this verification was done without at the same time verifying performance data for previous periods which had not been verified (October-December 2018 and January-March 2019). Finally, it is unclear why RBF payments for April-June 2019 had still not been made at the time of our study, despite that verification took place earlier in 2019. (Note: Further clarification on these issues would be useful).
Almost all health workers claimed that services provision continued as normal despite delays in RBF payments. But some planned activities could not be performed, and some community health workers were clearly demotivated. 98% of health workers claimed that service provision continued as before.
“They say you get paid based on your performance. Now you have worked, but the payment is delayed. You must somehow be affected, but that has not prevented us from continuing to provide service”. (Facility in-charge, Magu district council, Mwanza)
However, some activities were not performed as planned:
“There are areas where its implementation did not go as planned, for example (…) we planned to buy a solar panel and construct a fence for the incinerator and placenta pit, but its implementation was not done because RBF money was delayed” (Facility in-charge, Misungwi district council, Mwanza)
Many community health workers (CHWs) claimed they were fine with the delayed payments since they perceive themselves as volunteers and the RBF pay is just a bonus. However, some CHWs were clearly demotivated:
“It has affected us a lot even on how we work, we lost hope as we were dedicated and spent much time on the work, but the delays are too much for sure”. (CHW, Sengerema district council, Mwanza)
Some CHWs did not believe that lack of payment was due to delays, as they believed in-charges were holding their money.
Most health workers believed that payments would eventually arrive. This may have reduced the negative impacts on service delivery. 62% of health workers in Mwanza said they believed payments were delayed, while 38% believed that RBF had ended. Since most health workers believed that payments would eventually arrive, they still had incentives to perform well.
2.3 HBF-DHFF implementation
2.3.1 HBF-DHFF training
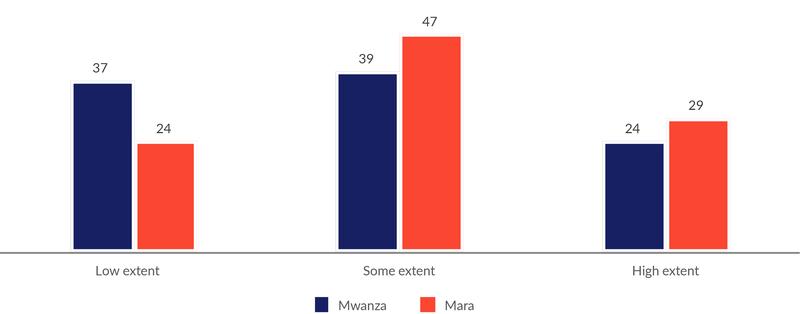
HBF-DHFF training was implemented as planned. However, a substantial share of facility in-charges found the training inadequate. Health workers and managers were trained in HBF-DHFF before implementation. This involved training in budgeting, planning and financial management, using PlanRep and FFARS. A significant share of facility in-charges claimed to have received inadequate training; 37% in Mwanza and 24% in Mara. Note that this is considerably higher than the share who reported inadequate training in RBF.
Short training time and lack of computer skills were key obstacles to receiving adequate training. Facility in-charges claimed to have a short time for training, which constrained the capacity to grasp the materials. The majority also found that the training on FFARS was challenging, as they lack prior computer skills.
2.3.2 HBF-DHFF payments
HBF-DHFF payments were largely made as planned, except for delayed disbursements for the last two quarters of 2019. Payments have been made as planned except for the last two quarters of 2019, which were delayed and disbursed in January-March 2020.
Delayed HBF-DHFF funds were reported to reduce service quality. Some facility in-charges highlighted how delays could negatively affect procurement of drugs and other activities:
“Delays like that result into the deficit that causes other services not to go on well at the facility, because in basket fund there is a percentage for medicine procurement and a percentage for other activities for the facility to carry on. When the clients come, they complain, and the service provider will try to explain but they [clients] don’t understand that things like delays can happen”. (Facility in-charge, Serengeti district council, Mara)
2.3.3 Implementation of e-systems (PlanRep and FFARS)
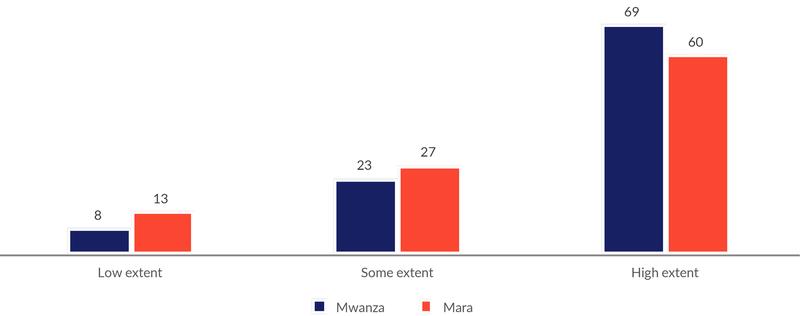
PlanRep and FFARS were largely implemented as planned, but some remote areas lack the power supply and internet required for their operation. FFARS and PlanRep were welcomed by the facility in-charges, as these systems strengthen transparency and accountability. In our facility survey, around two thirds responded that FFARS has worked as planned “to a high extent”, while around 10% responded “to a low extent”.
89% of the facilities reported that they use electronic FFARS while 4% use the manual version. 7% of the facilities claimed that they did not use FFARS yet (8 facilities in Mwanza and 3 in Mara).
However, reliable infrastructure for the e-systems is lacking in remote facilities.
“FFARS and PlanRep require the availability of a computer, strong and reliable internet, and electricity and network at the facility level. This has been a concern on the implementation side to most facilities in remote areas”. (Health Manager, Mwanza)
With regard to FFARS, there were no complaints if the staff had been trained properly. As one in-charge said, “It is a user-friendly system because it helps us a lot in accounting issues”. Some district and regional level managers had concerns about the capacity of local health facility staff to manage accounting and FFARS.
Deployment of facility accountants was seen as a crucial decision, but some dispensaries received inadequate support, perhaps due to limited financial resources to support visits by the accountants. As planned, health centres have employed accountants who offer support on financial matters to the health centre as well as nearby dispensaries. They are paid by their respective health centres. This was a crucial decision since most health workers lack financial management skills. However, in-charges of some dispensaries claimed to have received inadequate support from these accountants, partly because of insufficient budget/funds to pay for that support visit. These accountants are basically employed on temporary contracts and their salary payments are not reliably paid.
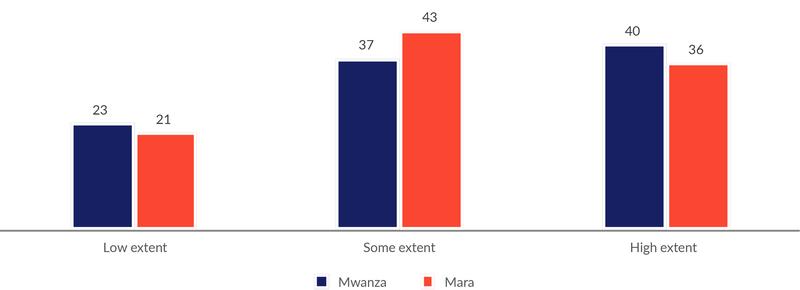
There is room for improvement in making active use of PlanRep in planning and budgeting. In our facility survey, 20% of in-charges said that they have used PlanRep to a low extent, while 40% had used it to some extent for planning and budgeting.
Some complained that PlanRep is not very user friendly and not inclusive of the data required. Others indicated that it is working well. As one RMO said, “And it has helped us a lot, as there is no over-expenditure, under-expenditure, and fund misallocation. Yeah and that’s major advantage of PlanRep, it has reduced a lot of queries and complaints about the basket fund.” This view was echoed at the facility level as well.
3. Obtaining and spending funds
3.1 Research questions and key findings
This chapter addresses the following research questions:
- What are facilities’ understanding of how RBF and HBF-DHFF funds are obtained?
- How have funds been flowing to the facilities through RBF and HBF-DHFF?
- How are RBF and HBF-DHFF funds budgeted and spent, and what is determining these decisions?
Key findings include:
- Most facility in-charges have a good understanding of how to obtain RBF funds, but more so in Mwanza than in Mara.
- Most in-charges also report that they are knowledgeable about how to obtain HBF-DHFF funds, but they seem to have significantly less confidence about these funds than about RBF funds.
- Facility in-charges demonstrated good knowledge about criteria for obtaining RBF funds. However, most in-charges were uncertain about payment criteria for HBF-DHFF.
- Budgeting and spending decisions with RBF have been ‘bottom-up’ and ‘needs-based’. HBF-DHFF budgeting and spending decisions have to a larger extent been ‘top-down’ and ‘rules-based’.
- RBF funds were first and foremost spent with the purpose of improving working conditions and quality of care. To increase service utilisation was a less prominent concern.
- Restrictions on how HBF-DHFF funds can be budgeted and spent were seen as a major constraint by a majority of facility in-charges.
- Regulations on how to use RBF funds were to a much lesser extent seen to restrict the facilities’ ability to improve service delivery.
- RBF funds and HBF-DHFF funds complemented each other, with RBF funds supplementing areas that HBF-DHFF could not cover or where funds were inadequate.
- Facilities used RBF resources to procure drugs and supplies and improve facility infrastructure based on facility priorities and needs.
- HBF-DHFF spending covered similar areas to RBF, but was more heavily and consistently focused on procuring medicines.
3.2 Understanding of how RBF and HBF-DHFF funds are obtained
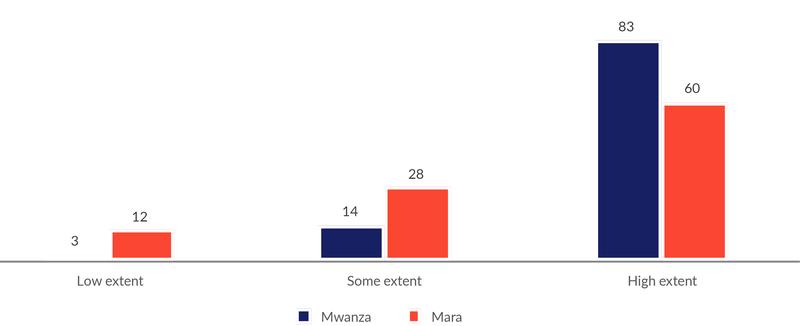
Most facility in-charges have a good understanding of how to obtain RBF funds, but more so in Mwanza than in Mara. In the health facility survey, 83% of the in-charges in Mwanza claimed that they ‘to a high extent’ know how to obtain RBF funds. This is significantly higher than in Mara (60%) (Figure 3.1). This difference might be explained by uncertainties related to the fact that Mara had not yet received any RBF funds.
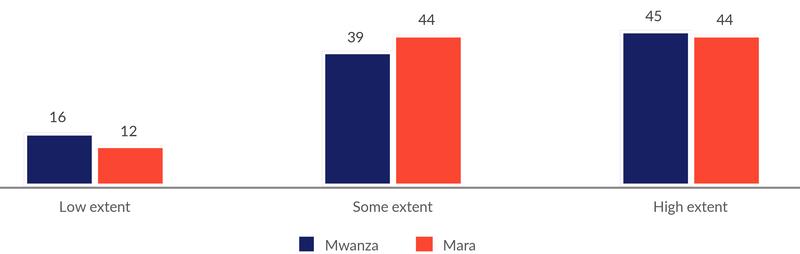
Most in-charges also report that they are knowledgeable about how to obtain HBF-DHFF funds, but their confidence seems to be significantly smaller about these funds than about RBF funds. Around 45% in each regions say that they ‘to a high extent’ know how to obtain HBF-DHFF funds (Figure 3.2). Around every 7th facility in-charge expresses limited knowledge on how to obtain HBF-DHFF funds.
Facility in-charges demonstrated good knowledge about criteria for obtaining RBF funds. In the qualitative interviews, the majority of respondents demonstrated knowledge on RBF indicators for payments as the key factor for receiving RBF money. Others mentioned the importance of accuracy in reported statistics, and how this differed between the funding systems.
“The difference which I saw is on the quality assurance [verification]; in RBF they consider quality assurance but in Basket Fund I don’t know. Until RBF is released there must be a verification, the verification team will come, they will do the verification and then will allow the payment, but I have not seen any verification team coming for Basket”. (Facility in-charge, Tarime district council, Mara)
However, most in-charges were uncertain about payment criteria for HBF-DHFF. Only a few mentioned catchment population size as a criterion for HBF, while others claimed that HBF has similar indicators to those of RBF.
“Basket fund money is allocated according to your catchment area and people you serve. That is what I know”. (Facility in-charge, Ilemela Town council, Mwanza)
“They [RBF and HBF] do not differ much because the criteria and components are in there, they do not differ greatly. If you improve in the RBF you will find it has also covered the Basket too in there”. (Facility in-charge, Magu district council, Mwanza)
3.3 How are RBF and HBF-DHFF funds budgeted and spent?
3.3.1 How budgeting and spending decision are made
Budgeting and spending decisions with RBF have been “bottom-up” and “needs-based”. HBF-DHFF budgeting and spending decisions have to a larger extent been “top-down” and “rules-based”. We noted a systematic difference in how budgeting and spending decisions were approached in the initial phase of RBF, and how such decisions are approached after the implementation of HBF-DHFF. While RBF budgeting and spending initially was guided by efforts to address specific needs at the facility, decisions under HBF-DHFF seem to a larger extent to follow from guidelines and protocols.
Following the implementation of HBF-DHFF, budgeting and spending categories are pre-determined in the electronic planning tools (PlanRep and FFARS) for both HBF-DHFF and RBF funds. This has reduced flexibility in RBF spending:
“Initially on RBF we used to spend according to our needs when we receive money, but now we are following the approved budget. If you planned to do something then you no longer have to enter something else, you must follow the budget that was approved”. (Facility in-charge, Sengerema district council, Mwanza)
It is conceivable that these technical changes might also weaken the ‘bottom-up’ and ‘needs-based’ approach to RBF budgeting, but our data does not allow for further exploration of this issue.
RBF funds were first and foremost spent with the purpose of improving working conditions and quality of care. To increase service utilisation was a less prominent concern. We asked in-charges in Mwanza to rate which concerns had been most important for how they had spent RBF funds. We gave them four options; the three that are mentioned in Figure 3.3, as well as ‘other concerns’, and they were asked to allocate four coins among the options as a way to rate their relative importance.
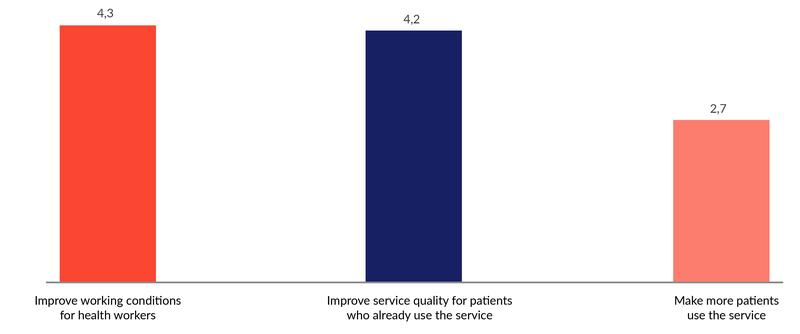
The main concerns have been to ‘improve working conditions for health workers’ and to ‘improve service quality for patients who already use the service’, while increased service utilisation has received significantly lower priority. These findings may be somewhat surprising in light of the RBF objectives which emphasise increased service utilisation. They are however in line with how health workers have talked about the benefits of RBF in our earlier process evaluations. One possible explanation is that increased utilisation not only represents benefits (higher bonus) but also costs (higher workload), while there are lower—or no—such costs related to the other items.
Restrictions on how HBF-DHFF funds can be budgeted and spent were seen as a major constraint by a majority of facility in-charges. Some in-charges reported frustration that basket funding could not be budgeted to pay for construction work as well as expenses such as allowances to doctors on call and payment of casual labourers. They asked for greater autonomy in deciding how to spend money and respond to emerging challenges that were not foreseen in the annual plans, and they complained about limited flexibility to change items in response to changing needs.
“(…) sometimes the money is there but there is something you have to prioritise but because it was not on the budget during planning then you may not implement it […]” (Facility in-charge, Kwimba district, Mwanza)
“There is an action plan and everything is ready, they have already [been] allocated; if 50% is supposed to go to medicine then it should go there, if it is hospital supply it should go there. I mean you cannot take money here and use for construction…”. (Facility in-charge, Sengerema district council, Mwanza)
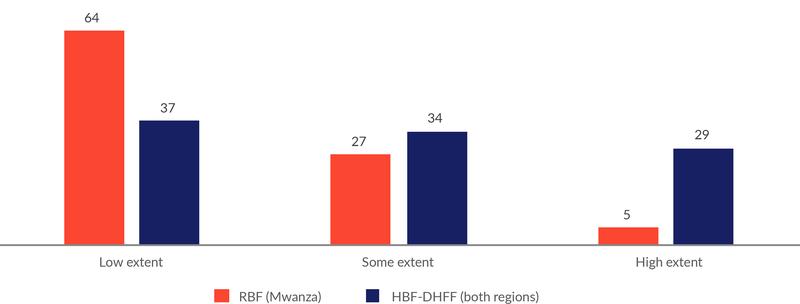
Regulations on how to use RBF funds were to a much lesser extent seen to restrict the facilities’ ability to improve service delivery. While a majority of the respondents in the health facility survey thinks that regulations on HBF-DHFF funds are somewhat or highly restrictive, the opposite is the case for RBF funds (Figure 3.4).
*Note: 4% of facility in-charges in Mwanza answered ‘not applicable’ to the RBF question.
3.3.2 What the funds are spent on
Facilities used RBF resources to procure drugs and supplies and improve facility infrastructure based on facility priorities and needs. Drugs that were out of stock were often procured using RBF resources together with medical equipment such as blood pressure machines where these were broken or unavailable and computers to improve the storage of medical records. Priority was generally given to medicines that related to the delivery of RBF incentivised services such as iron tablets, SP, and Vitamin A. Investments were also commonly reported in facility infrastructure, including furniture such as chairs, tables, benches, cupboards, labour beds, and door handles. Facility repairs were undertaken where needed. Investment in utilities and waste disposal were also widely cited, such as solar panels for electricity, water tank systems, and gutters for harvesting rain water. Providers indicated that the main rationale for their investment choices was to ensure they met the standards for RBF enrolment and thereafter to perform better in relation to incentivised services, and to ensure they were able to offer services such as deliveries and perform routine tests to avoid referring to the district hospital.
“[It] depends on the needs of the health facilities, for example when RBF started many facilities didn’t have incinerators or placenta pits […] many facilities didn’t have benches for patients to sit while waiting for services, notice boards, suggestion boxes so they bought all those. They came to water sources, they made sure each facility that did not have a source of water bought sim-tanks for harvesting rainwater. They came to electricity; many health facilities did not have electricity, so they installed electricity and others solar power.” (District level stakeholder, Misungwi district, Mwanza)
HBF-DHFF spending covered similar areas to RBF, but was more heavily and consistently focused on procuring medicines. This was to ensure drugs and supplies were not out of stock (as 33% of spending is to be in this category). Other areas of investment included the procurement of gas tanks and gas refills to store vaccines, funding for emergency transport for safe referral for delivery and airtime for staff. HBF-DHFF funds were also used to pay per diems to health facility governing committee members to attend meetings.
“Most of basket money goes to drug supply, this is the first priority when most of the money goes there. Drug supply and another area is action plan when budget is brought at the end of the year.” (Facility in-charge, Sengerema district, Mwanza)
RBF funds and HBF-DHFF funds complemented each other, with RBF funds supplementing areas that HBF-DHFF could not cover or where funds were inadequate. For example, renovations were cited as an area that HBF-DHFF did not support. It was strongly felt that these two funding streams supported each other.
“(…) there is no place you can say RBF money can cover everything, it has never happened to be honest, because RBF money finishes, and you take some out from Basket Fund that’s why I say in general they depend on each other.” (Facility in-charge, Kwimba district, Mwanza)
4. Effects on service delivery and governance
4.1 Research questions and key findings
This chapter addresses the following research questions:
- How have RBF and HBF-DHFF affected the delivery of services?
- What factors have facilitated or inhibited positive impacts of RBF/HBF-DHFF on service delivery?
- How have RBF and HBF-DHFF affected governance and accountability mechanisms?
Key findings on service delivery in relation to RBF include:
- Statistical analysis of administrative data suggests that RBF had a significant positive impact on service utilisation of many incentivised services, especially those relating to maternal health, with most effects taking place after the introduction of HBF-DHFF.
- The delay in RBF payments from end-2018 does not seem to have seriously impacted service utilisation.
- The availability of drugs and supplies increased significantly between 2016 and 2020 in both regions, and more so in Mwanza than in Mara.
- Perceived changes contributing to improved service delivery:
- Improvement in the morale of health workers and their ability to do their job.
- Health workers were more ‘client orientated’ as they directly associated patients with additional money.
- A reduction in absenteeism among health workers, together with greater efficiency of work undertaken.
- Greater teamwork and use of data and improvements in the functioning of facility governing committees.
- Supervision became more results-focused.
- More facilities made efforts to boost demand for delivery care.
- Perceived changes not contributing to improved service delivery:
- RBF focused attention on some services to the detriment of others and gave incentives to misreport results to obtain a higher bonus.
- In some cases, facilities competed with each other for patients rather than working together to support their care.
- The main design features associated with the positive effects of RBF were the additional funding, the incentives for health workers and facilities, the verification visits and performance monitoring, and the increased autonomy and control over funds and their use.
- RBF design features contributing negatively included inequities in the allocation of bonuses, the omission of governing committees as a bonus beneficiary and a disconnect between the level of bonus and the level of effort made.
- Contextual factors reported to limit the effect of RBF included: staffing shortages, insufficient health worker training, access barriers for patients, and a lack of community health awareness.
- Other challenges identified by respondents include concerns about long term sustainability of the programme.
Key findings on service delivery in relation to HBF-DHFF include:
- Improved work environment, particularly through reduced drug stock outs. Still, the perceived impact of HBF-DHFF on the availability of drugs and supplies was not as strong as the impact of RBF.
- Enhanced provider autonomy by giving providers responsibility for budgeting and managing funds at the facility level.
- Reduced need to pass through bureaucratic processes to access funds.
- Increased capacity to attract community health fund (CHF) members, due to the improved availability of drugs and supplies at the facility.
Key findings relating to governance include:
- Both RBF and HBF-DHFF have resulted in more frequent HFGC meetings and greater involvement of HFGC in budgeting and spending decisions.
- RBF and HBF-DHFF increased HFGCs’ “voice” and influence on facility functioning.
- Planning the use of funds and transparency in funding allocation have empowered HFGC members; lack of capacity of committee members is a constraint.
- RBF and HBF-DHFF have created new forms of mutual dependency between facilities and the district level.
- Greater transparency around the allocation of basket funds has improved providers’ attitudes towards district managers and reduced conflict within the district; however, some district managers were unhappy about their loss of power, and there were constraints to visiting facilities in some areas.
4.2 Effects on the organisation and delivery of services
4.2.1 Service utilisation
Statistical analysis suggests that RBF had a significant positive impact on service utilisation of many incentivised services, especially those relating to maternal health, with most effects taking place after 2018.
This section describes trends in the utilisation of health services based on routine administrative data (DHIS2). We also estimated programme effects using difference-in-difference regression models, the results of which are shown in the Appendix. We have conducted analyses on 12 of the 16 services incentivised by RBF. (See more on methods in Section 1.5.3.)
RBF had a significant positive impact on service utilisation of many incentivised services, especially those relating to maternal health:
- ANC consultations before 12 weeks of gestation
- At least four ANC visits
- IPT2 for pregnant women
- Institutional deliveries
- Postnatal care within 3-7 days
- OPD visits
- Use of modern contraceptives
- HIV counselling and testing
For the remaining four indicators there was no statistically significant change (using a 5% level of significance).
One potential weakness of using administrative data is that reporting completeness may improve as a result of RBF, which may bias estimates upwards. However, there seems to be little reason to be concerned about such effects here, as there was no sudden positive jump in indicators when RBF started. Rather, the figures below suggest that it took time for the effects of RBF to materialise. Indeed, for only two of the indicators were there significant effects detected before 2018. Note, however, that these estimates are quite conservative as they put the same weight on all quarters from the start of RBF, while there are several reasons for believing that effects happened more gradually (see methods section in Chapter 1).
The fact that most of the effects of RBF seem to have taken place after 2018, when also HBF-DHFF was implemented, can be interpreted in several ways. First, it is possible that it simply took time for RBF to make an impact. Second, it is possible that there was a positive synergy between RBF and HBF-DHFF which led to a bigger and faster increase in service utilisation in Mwanza where RBF was already implemented. It is conceivable that facilities in Mwanza were better able to take advantage of HBF-DFF due to their prior experience with direct facility financing through RBF. However, as will become clear from the discussion below, there are indications in the data that the gradual effect of RBF started before the implementation of HBF-DHFF, which lends support to the former explanation, i.e., a delayed effect.
Another noteworthy observation is that the stop in RBF payments in Mwanza from end-2018 does not seem to have seriously impacted service utilisation.
The more detailed discussion below presents the estimated impact of RBF on each service indicator. The percentage change is measured relative to the average performance in Mwanza in the five quarters before the implementation of RBF, i.e., from the beginning of 2015 to the end of first quarter 2016.
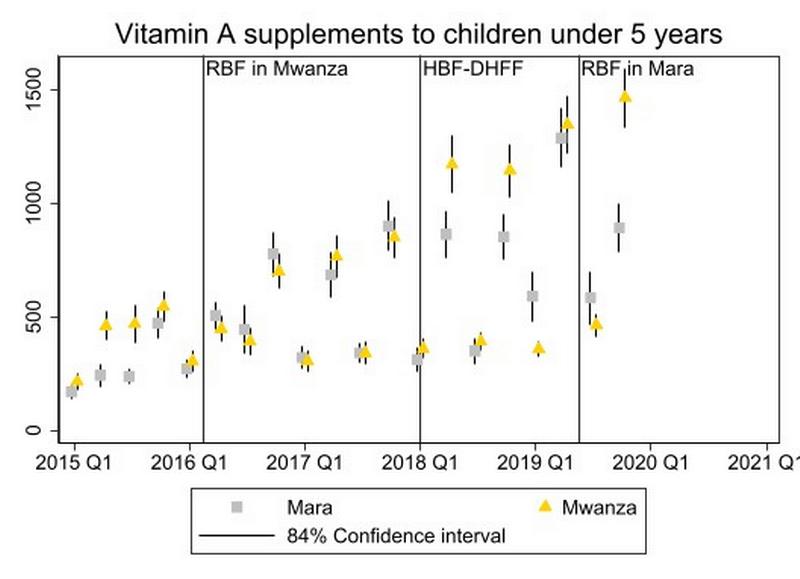
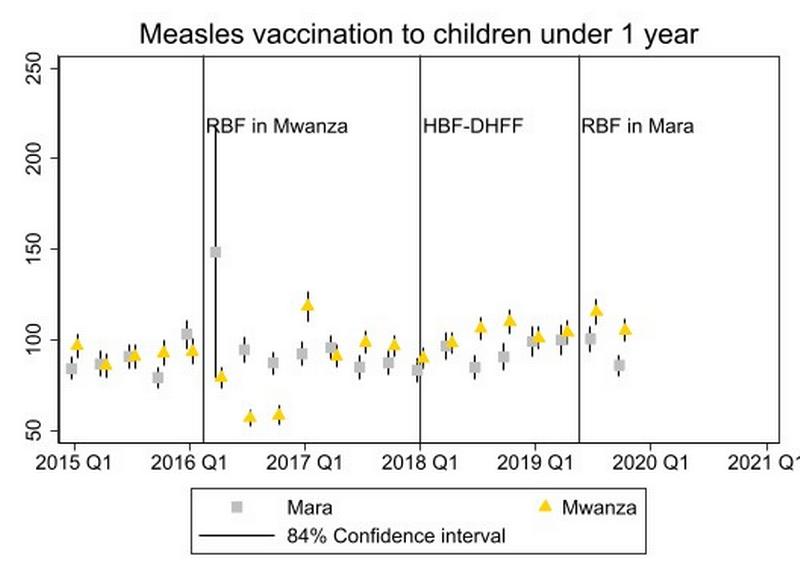
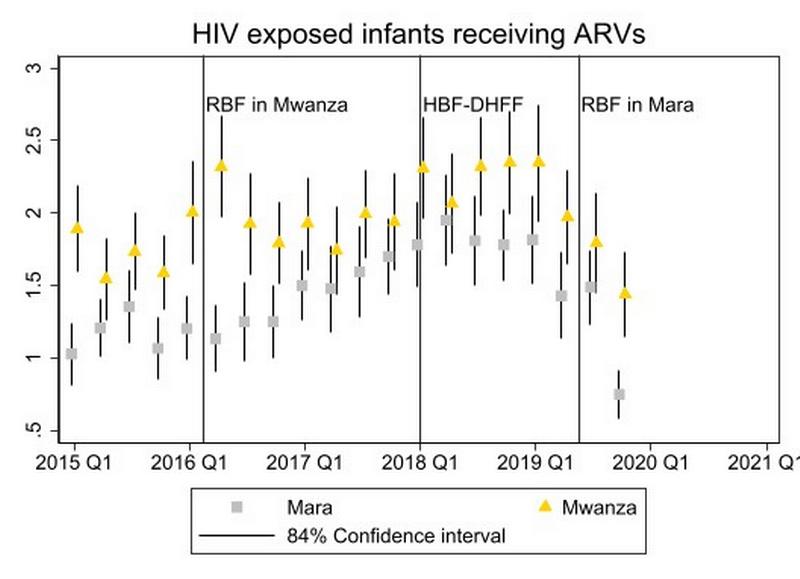
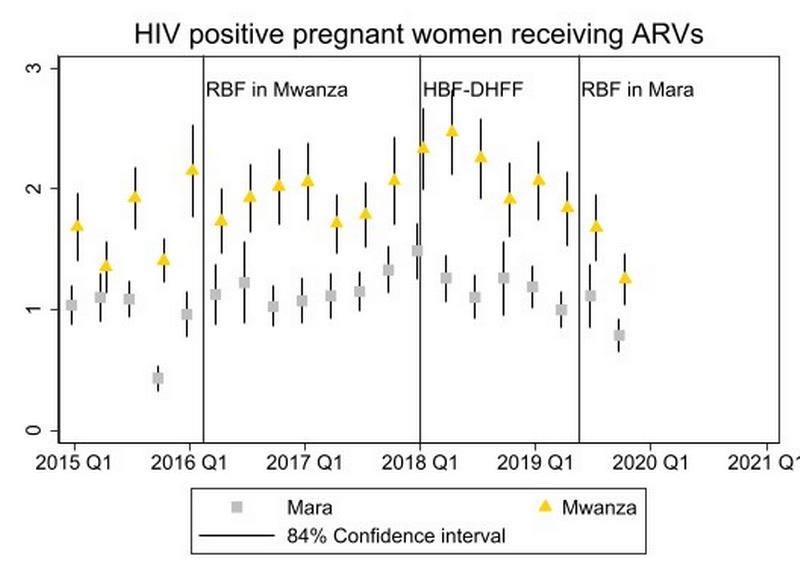
Guide to reading the graphs: Each data point represents the average number of services provided in each quarter, with yellow colours for Mwanza and grey for Mara. The vertical lines at each data point represent the confidence interval. We used the 84% confidence interval since this has a straightforward interpretation; if the lines attached to two different data points do not overlap, there is a statistically significant difference between those observations. The three vertical lines mark when the financing reforms started; first RBF in Mwanza, then HBF-DHFF in both regions, and finally RBF in Mwanza. (See methods section above for a further discussion.) We included utilisation data from before the implementation of RBF to assess whether service utilisation was similar in the two regions at baseline, and most importantly, whether the trends in service utilisation were parallel or not. If trends are parallel before the intervention, there is increased likelihood that the difference-in-difference estimation provides unbiased estimates of the effects of RBF.
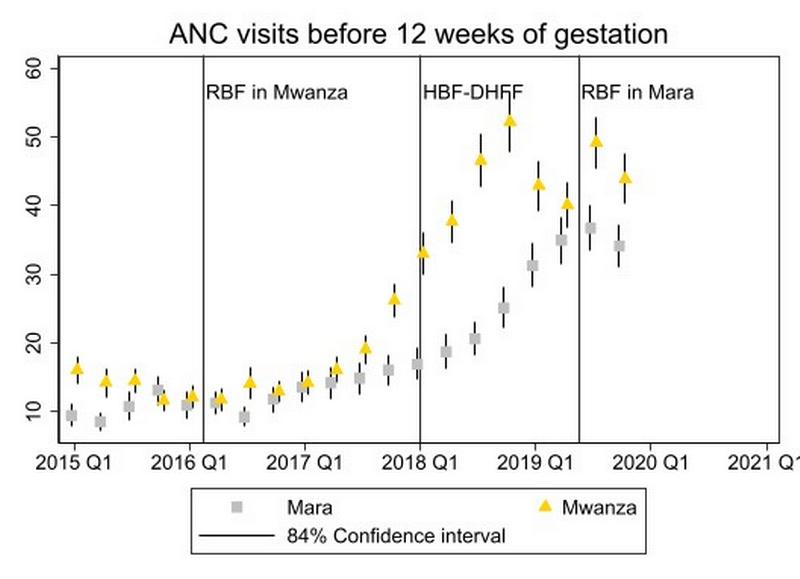
There has been a strongly increasing trend in ANC visits before 12 weeks of gestation in both regions since 2017/18, but more so in Mwanza than in Mara. The increase in Mwanza started before the implementation of HBF-DHFF, although there is no statistically significant impact of RBF for this early phase as a whole. Estimated effect of RBF: 67% (p<0.01).
Note that the trends were not parallel at the outset, but with a negative trend in Mwanza and a positive in Mara, the true effect of RBF is likely to have been even larger than our statistical analysis suggests.
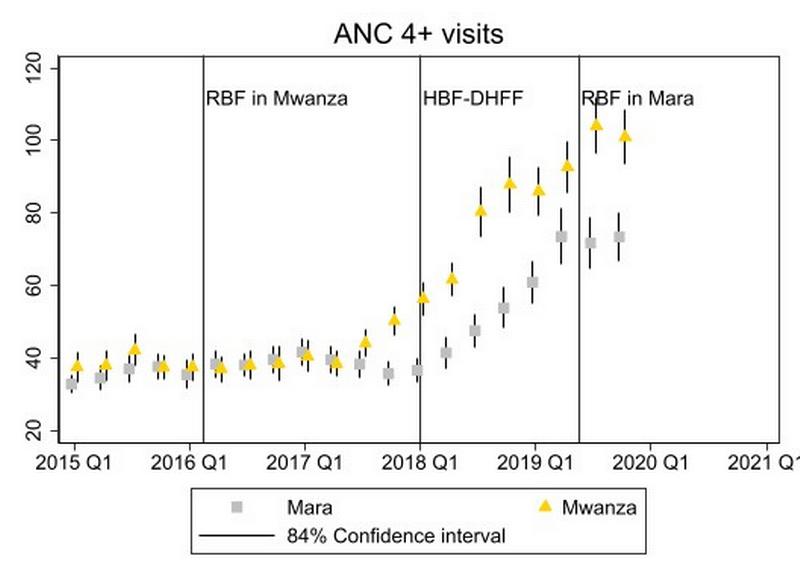
The number of pregnant women with at least four ANC visits has evolved along the same pattern as the number of early ANC visits.
Estimated effect of RBF: 29% (p<0.01).
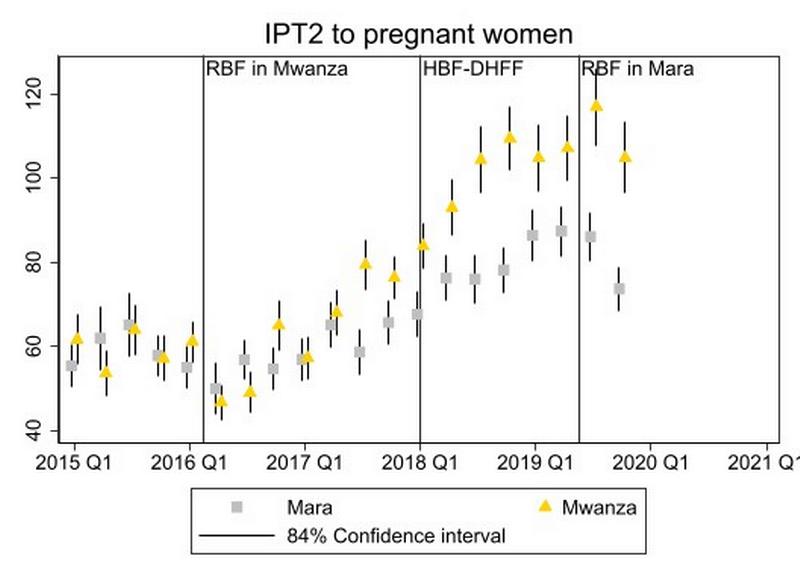
IPT2 to pregnant women also shows a somewhat similar patterns to the above indicators, which is natural since this service is provided as part of ANC consultations. Also note that the increase in Mwanza above Mara seemed to start before the implementation of HBF-DHFF, although there is no significant effect for the whole of this early phase.
Estimated effect of RBF: 17% (p<0.001).
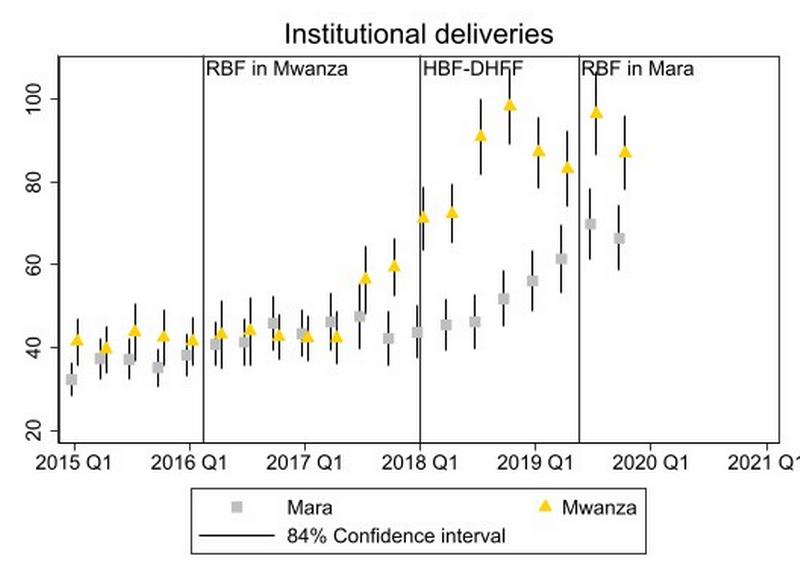
The data on institutional deliveries also shows the same pattern as the data on ANC utilisation. The same underlying mechanisms may be at work for all these services.
Estimated effect of RBF: 32% (p<0.01).

Again, we observe the same pattern. Overall, there is a quite consistent pattern suggesting that RBF has increased the utilisation of maternal health services.
Estimated effect of RBF: 111% (p<0.01).
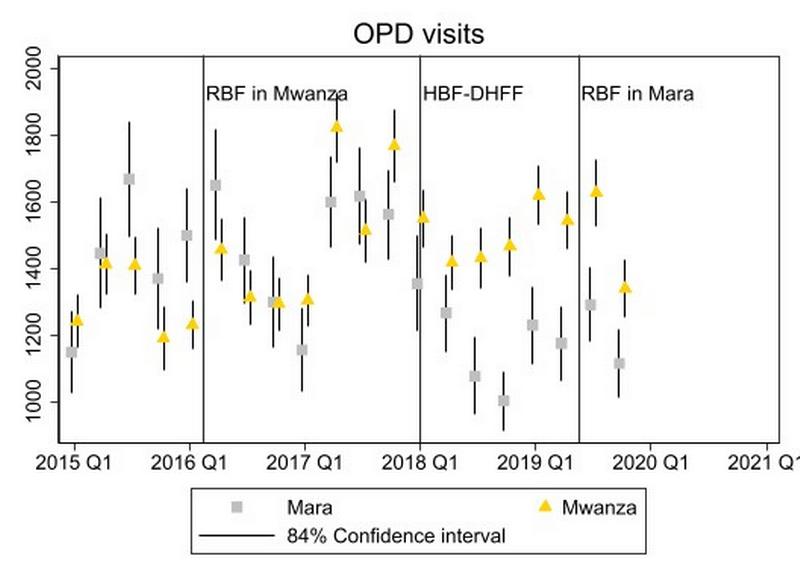
The pattern for OPD visits differs markedly from the maternal services discussed above. The volatility is much higher, perhaps reflecting seasonality and outbreaks of various infectious diseases. Such outbreaks may have affected the two regions differently, which should make us careful in drawing strong conclusions based on our analysis. Nevertheless, the statistical analysis shows a positive effect of RBF.
Estimated effect of RBF: 22% (p<0.01).
Note that in this case, pre-trends are not parallel, but since the trends are negative in Mwanza and positive in Mara, our effect estimate is most likely biased downwards.
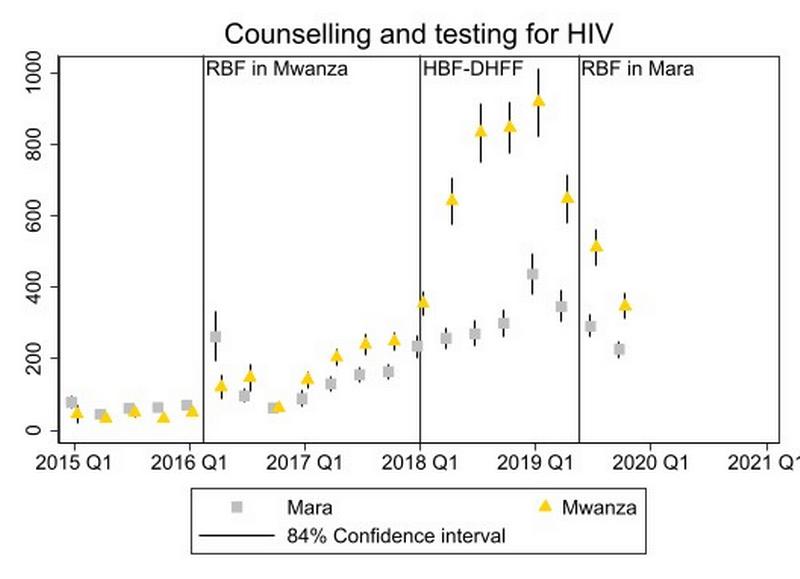
There was a remarkably big jump in the number of clients counselled and tested for HIV in Mwanza from 2018 onwards. For this indicator, there is in fact also a significant positive effect also in the early phase before implementation of HBF-DHFF, though this effect is much smaller than for the full period.
Estimated effect of RBF: 533% (p<0.01).
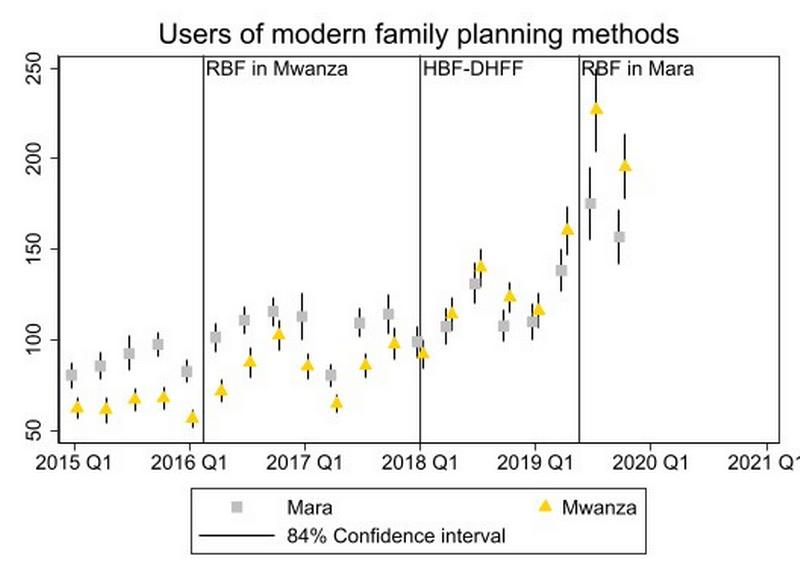
The statistical analysis also shows a positive effect on the use of modern planning methods. However, the pattern here is quite different from the indicators below. What seems to have happened here is that Mwanza started out lower than Mara and has caught up.
Estimated effect of RBF: 27% (p<0.01).
The patterns for the remaining four indicators are shown below. The estimated effect of RBF was not statistically significant at the 5% level for any of these indicators. When it comes to Vitamin A supplementation, while data are quite erratic, there seems to be an overall trend towards higher provision of this service in both regions, and the estimated trend is in fact a bit more positive in Mara than in Mwanza. Hence, these changes are likely explained by other factors than RBF. Regarding measles vaccination, it should be noted that vaccination coverage was close to 90% in both regions during the last Demographic and Health Survey (2015/16), and the scope for improvement was therefore limited. Finally, the number of mothers and children receiving HIV services seems to be stable at a low level.
The delay in RBF payments from end-2018 does not seem to have seriously impacted service utilisation. This may appear somewhat puzzling in light of the importance attributed to additional resources in improving service delivery (see section 4.3). One potential explanation is that service demand is sticky: although the quality of services may have declined somewhat, it takes time to reduce service demand, just as it took time for RBF to increase service utilisation in the first place. Moreover, the implementation of HBF-DHFF may have contributed to maintain the quality of services through its positive effect on drug supply (see more below). Finally, most health workers continued to believe that they would eventually receive their bonuses, which implies that the incentive mechanism was still in effect even though payments were delayed.
4.2.2 Drugs and supplies
The facility survey shows that the availability of drugs and supplies increased significantly between 2016 and 2020 in both regions, and more so in Mwanza than in Mara. Table 4.1 shows the number of drugs, supplies, contraceptives, and functional medical equipment available at the day of visit at baseline and endline. There was an improvement in all categories in both regions (although the increase in contraceptives in Mara was not statistically significant).
A star (*) means that the increase was statistically significant at 5% level.
Further analysis shows that the improvement in availability of drugs and medical supplies was stronger in Mwanza than in Mara.
These results, together with the qualitative findings presented below, provide suggestive evidence that both RBF and HBF-DHFF have contributed to improved availability of drugs and supplies. Improvements in Mara are likely caused at least partly by HBF-DHFF and not by RBF since there have been no RBF payments yet. A larger improvement in Mwanza than in Mara suggests that RBF has an impact beyond the improvement caused by HBF-DHFF.
4.2.3 Perceptions of the impact of RBF and HBF-DHFF
This section presents how health workers and health managers perceive the impacts of RBF and HBF-DHFF on service delivery. Since it is in the personal interest of many of these stakeholders to maintain these funding mechanisms, findings should be interpreted with care.
Perceived RBF effects
A variety of positive effects of RBF were noted by respondents in relation to service delivery, both on the demand and the supply side. These effects were fairly consistent across districts in both Mwanza and Mara region, despite the fact that facilities in Mara region had not yet received any RBF funds.
RBF improved the morale of health workers and their ability to do their job. Previously, a lack of resources had sometimes constrained providers’ ability to do their job, whereas RBF had allowed gaps in service delivery to be identified and overcome through investments in drugs and supplies and facility infrastructure. Improvements in the management and completeness of data were also reported to have been a help in motivating health workers, by helping to see their progress and where further improvements were needed. Greater knowledge levels, especially in relation to data management and reporting, together with reporting on income and expenditure, were also reported.
RBF made health workers more ‘client orientated’ as they directly associated patients with additional money. This resulted in more kindness and supportiveness towards patients and their needs.
“It changed the staff first […] it changed employees’ attitude of seeing a customer as something to just come […]if you contempt them you will not earn money. […] it made us change and care more for our patients.” (Facility in-charge, Kwimba district, Mwanza.)
Stakeholders frequently mentioned a reduction in absenteeism among health workers, together with greater efficiency of work undertaken. Competition between health facilities was highlighted as a further motivating factor, as they wanted to do well compared to neighbouring facilities and ensure they attracted more patients. In some facilities, controls had been introduced to monitor health worker presence at facilities. However, our quantitative health worker survey detected no significant programme effect on hours worked or absenteeism.
Greater teamwork. RBF led to doctors offering support to under-resourced service areas outside of their usual remit (noted in Magu district). Some facilities reported daily briefing meetings among staff to discuss challenges, review suggestions made by patients and implement solutions.
“(…) since this project has been introduced, we found ourselves no longer working individually; you find we have created some kind of connection between us.” (Facility in-charge, Ukererwe district, Mwanza.)
Supervision became more results-focused, as RBF made supervisors focus their attention on performance gaps and how to improve performance.
The health worker survey found that almost all facilities had introduced strategies to boost demand for delivery care with the most common strategies being to encourage community health workers or traditional birth assistants to bring women to the facility, and to provide more prompt attention to women at the facility. In both regions, such strategies were used much more frequently at endline than at baseline, and the data does not provide any evidence that the increase was larger or smaller in one region compared to the other.
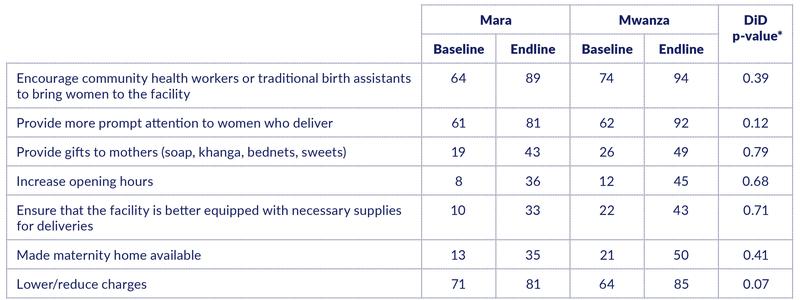
Note: The difference-in-difference (DiD) p-value is the probability of the observed data, given that in reality there was no greater change over time in Mwanza than in Mara. A p-value less than 0.05 indicates a statistically significant programme effect.
Strategies for increasing the number of OPD patients were less common. But the share of facilities pursuing such strategies have increased strongly in Mwanza, from 17% at baseline to 45% at endline. The increase is significantly larger than in Mara. This may be somewhat surprising because HBF-DHFF has been implemented in Mara for several years, with OPD visits as the only incentivised indicator. This may suggest that HBF-DHFF has not made facilities focus explicitly on increasing service utilisation.
Some negative effects of RBF were also noted. RBF focused attention on some services to the detriment of others and gave incentives to misreport results to obtain a higher bonus. OPD services were reported to receive less attention compared to maternal services, for instance, even though OPD services also were incentivised.
“At the beginning when RBF commenced, people woke up and experienced benefits; some activities not relating to RBF indicators got paralyzed.” (Magu district stakeholder, Mwanza.)
“(…) there are some people who can cheat and put a high number of patients so as to receive a lot of money.” (Facility in -charge, Misungwi district, Mwanza.)
In some cases, facilities competed with each other for patients rather than working together to support their care.
Perceived HBF-DHFF effects
The basket funding was seen to have improved the work environment, particularly in relation to reducing drug stock outs. Facilities consistently reported that drug stock outs were no longer a problem due to HBF-DHFF.
“The basket fund has pushed us so much in terms of accessibility of medicines. We buy medicine, and it also makes it easier for us to operate the facility.” (Facility in charge, Serengeti district, Mara.)
In Mwanza region it was also reported that outreach activities had raised community awareness and trust, boosting demand especially for maternal and child health services and vaccinations.
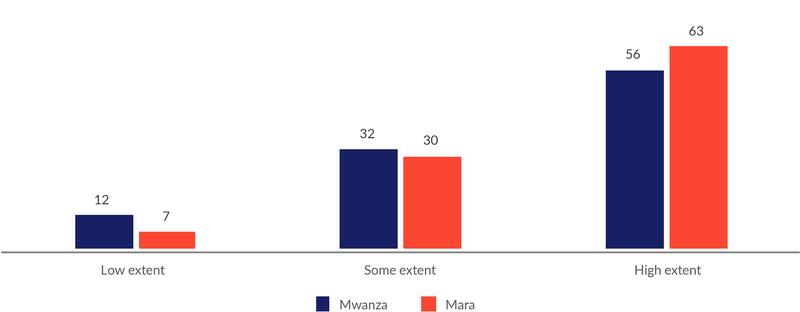
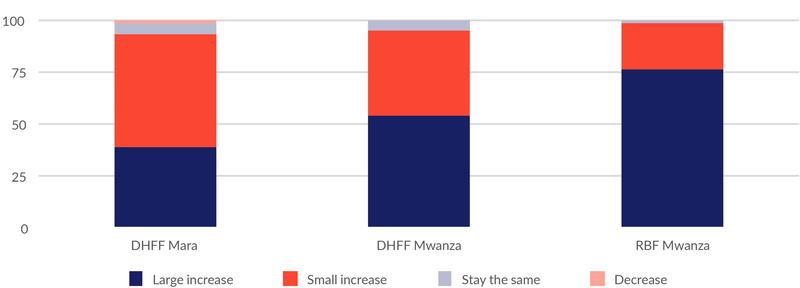
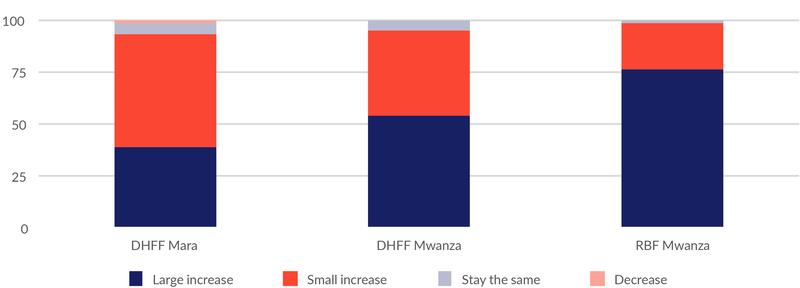
The impact of HBF-DHFF on the availability of drugs and supplies was perceived to be not as strong as the impact of RBF. Almost all health workers reported both sources of financing had increased the availability of drugs and supplies, but a higher proportion reported that there had been a large increase due to RBF compared to HBF-DHFF (76% vs. 54% in Mwanza, see Figure 4.1).
HBF-DHFF was seen to have 1) enhanced provider autonomy by giving providers responsibility for budgeting and managing funds at the facility level and 2) reduced the need to pass through bureaucratic processes to access funds.
“The positive impacts that we got is that (…) we don’t depend much on or waste a lot of time waiting for the higher administrators to support us and keep the patients waiting too.” (Facility in-charge, Ukererwe district, Mwanza.)
“DHFF has increased (…) the sense of ownership of the things which they (health workers) are doing, because they know that they are the ones who wanted that thing, this is different from when the plans come from us (Health managers) and they just implement.” (District stakeholder, Misungwi district, Mwanza.)
Some facilities felt that the basket fund had increased their capacity to attract community health fund (CHF) members, due to the improved availability of drugs and supplies at the facility.
”I can say it [DHFF] has added a lot of CHF insurance clients , because if medicines are available, [and] medical supplies, you find they come to you” (Facility in-charge, Rorya district, Mara.)
4.3 Factors that facilitated or inhibited change in service delivery
4.3.1 RBF design and RBF effects
The main design features associated with the positive effects of RBF were the additional funding, the incentives for health workers and facilities, the verification visits and performance monitoring, and the increased autonomy and control over funds and their use. When asked which aspects of the RBF design contributed to the programme’s effects on service delivery, almost all those interviewed pointed to the fact there were more resources available for health workers, which was motivating to them. They also highlighted the additional facility resources, which improved the work environment. Verification, performance monitoring, identifying and resolving bottlenecks were also seen to be significant factors explaining the positive effects of RBF independently of the additional financial resources. Lastly, providers pointed to the increase in autonomy and control over funds and how to spend these as a key element underpinning the success of the RBF programme.
“Because spending RBF money is our responsibility, no one interferes with us, but you spend the money based on your plans, that is one.” (Facility in-charge, Misungwi district, Mwanza.)
We asked facility in-charges to rank the importance of the various RBF design elements according to their importance in improving service delivery. They were given 18 coins that they could allocate to nine different design elements. As shown in Figure 4.2, they ranked the resource effects (additional resources for facilities) the highest, followed by incentives for facilities and health workers. The “softer” elements of the RBF scheme, such as greater autonomy, more involvement of governing committees, and more support from the district level, ranked lower. Interestingly, higher health worker pay ranked one of the lowest, whereas the monetary incentives for health workers were ranked highly. The natural interpretation is that higher health worker salaries would not improve services to the same extent as performance pay.
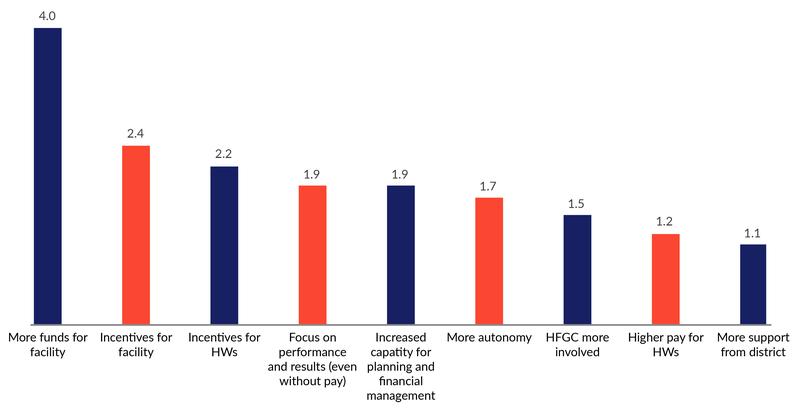
Negative design features included inequities in the allocation of bonuses, the omission of governing committees as a bonus beneficiary and a disconnect between the level of bonus and the level of effort made. Specific concerns included inequities in the way bonuses were allocated. The fact that the health facility governing committees did not receive bonus payments and had not been trained about RBF, yet were required to be signatories on RBF spending, caused tensions in the relationship with health workers at times.
“Especially on the matter of withdrawing the 25% which also requires the committee’s approval, (…) they always appear upset on this matter as they think they deserve some amount of it, too. (…) They kind of feel inferior, I don’t know how to put it, but it hurts them.” (Facility in-charge, Ukererwe district, Mwanza.)
Others pointed to the differential bonus by cadre, which did not always reflect effort made. It was also highlighted that the RBF coordinator was not considered in the responsibility points at the district and regional level.
“(…) during payments they consider education and your position. Let’s say, because you are facility in charge [you] will get 100%, now come to the leading one, the RN or EN at facility, tasks performed are twice as much as the one receiving 100%. This is still a hot debate to date; they ask when shall you change those issues?” (Magu district stakeholder, Mwanza.)
Other challenges identified by respondents include concerns about long-term sustainability of the programme. Two respondents also raised concerns about the longer-term effects of RBF once incentives are removed, and how that might affect motivation in the future.
“if (…) workers (are) thinking only about money, we won’t be able to sustain it, the good services, because these are projects, and whenever the project ends, people are just focused on getting the extra pay, we won’t be able to sustain for long. (…) I feel if people just think about getting extra income and they are not getting it anymore, the situation will not be so good.” (Regional stakeholder, Mara region.)
4.3.2 Contextual factors
The following contextual challenges were identified by respondents as limiting RBF effects: staffing shortages, insufficient health worker training, access barriers for patients, and a lack of community health awareness. Concerns about staffing shortages were expressed by a number of facilities, and in one case it was also perceived that health workers were not getting sufficient training before being posted to facilities; hence their capacity for service delivery was limited. Facilities reported challenges getting more patients during the rainy season or in island settings and where there is heavy concentration of providers in their locality, which limited their ability to get bonus payments.
“(…) [we] cannot get same results like those that offer service to two or more villages. While we only serve 900 houses of only one village, (…) others have more than 900 houses. [It] means they will always score higher on those indicators.” (Facility in-charge, Ukerewe district, Mwanza.)
Low levels of awareness and education in the community were identified as a further challenge, although it was reported that home visits and outreach activities by CHWs were offsetting this. Some facilities reported that CHWs had faced barriers gaining acceptance into the community unless accompanied by village leaders.
4.4 Effects on governance and accountability
4.4.1 Effects on Health Facility Governing Committees (HFGCs)
Both RBF and HBF-DHFF have resulted in more frequent HFGC meetings and greater involvement of HFGC in budgeting and spending decisions, with increases in the frequency of meetings noted in both regions between 2016 and 2020. The increase in number of meetings during the prior 12 months was higher in Mwanza (from 3.4 meetings in 2016 to 5.7 in 2020) than in Mara (from 3.8 meetings in 2016 to 5 in 2020).
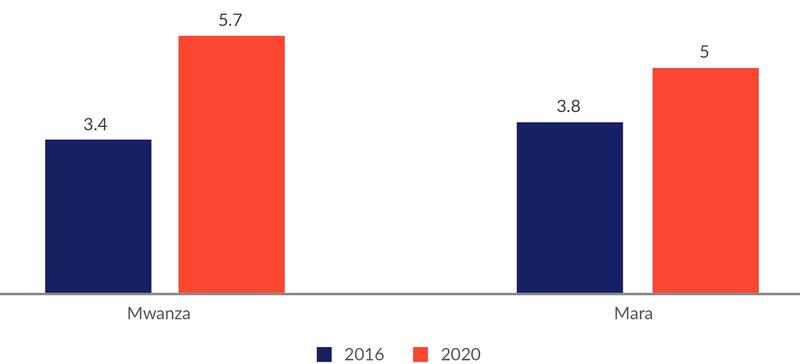
High degree of participation of HFGCs in the planning/budgeting and spending of funds was also reported (Figure 4.4.) For RBF we asked to which extent HFGCs participated in spending decisions, while for HBF-DHFF we asked to which extent they participated in planning and budgeting. The figures are therefore not directly comparable.

A facilitating factor for this increase and high level of participation is that several members of HFGCs indicated that HBF-DHFF provides allowances to HFGC members, which motivates participation in meetings. However, RBF funds were not used in this way, which led to reports that HFGCs lack funds to support their work.
RBF and HBF-DHFF increased HFGCs’ “voice” and influence on facility functioning
The interviews reveal that the HFGCs reported the feeling that they “own” the facilities. This was positive; the sense of “ownership” gave the HFGCs a feeling of confidence and control.
“It has built up the health facility governing committee’s capacity and confidence. So, the facility has become theirs and they have power to make decisions on their facility, but the other thing is the circle has been shortened in a sense that they can make decisions directly without being interfered with by CHMT [Council Health Management Team] and councilors.” (District level stakeholder, Tarime DC, Mara.)
The survey with facility in-charges also suggested that the HFGCs have experienced a significant increase in their influence on health facility planning during the last four years. In Mwanza, 67% said that HFGC has had “much more influence”, while 27% responded “somewhat more influence”. The pattern was similar in Mara (see figure below).
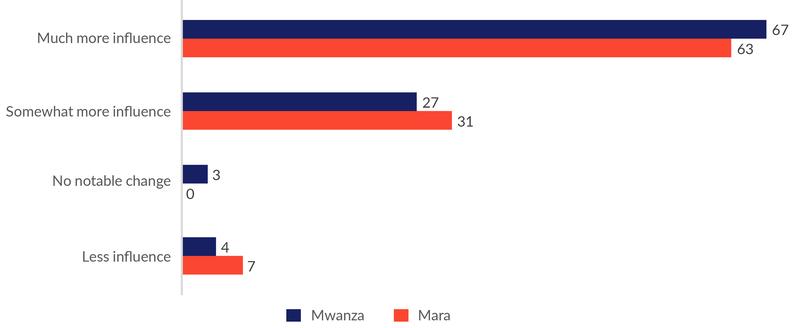
Autonomy to plan the use of funds and transparency in funding allocation have empowered HFGC members, but lack of capacity of committee members is a constraint.
Autonomy enabled HFGCs to plan the use of funds to meet identified needs, and the use of FFARS resulted in greater transparency within facility on the flow and allocation of funds and contributed to more democratic decision making. One inhibiting factor is that the HFGCs operate under constraints of human capacity and limited know-how. A district medical officer said, “They don’t understand the data”. The use of accountants has helped quite a lot, though.
4.4.2 Effects on the relationships between district managers and health facilities
RBF and HBF-DHFF have created new forms of mutual dependency between facilities and the district level. In the case of RBF, mutual dependency is built into the structure of the scheme. District level managers depend on performance of facilities for bonuses, while health facilities rely on district level managers for technical knowledge to manage finances and achieve performance targets. One in-charge indicated that the support from the district level managers improved health worker motivation under RBF, which resulted in changes that attracted more clients to the health facility and increased their earnings.
HBF-DHFF also increases health facilities’ need for technical support from the district level, in particular when they have limited capacity themselves for financial management, and all health facilities rely on district managers for authorisation of payments. The dependency of district level managers on health facilities is less obvious, as there are no bonuses for district level staff as in RBF. However, similar systems seem to have emerged under HBF-DHFF as health facilities use their funds to pay allowances for districts level managers for their technical support. Many health facilities reported that district level managers have been invited to conduct capacity building coaching workshops with health workers on a particular topic. This increases the visibility and contact time between the health facilities and district managers in a supporting environment, which contributes to their improved relations. The ability of facilities to pay allowances to travelling district managers is a potentially important mechanism for balancing the power that the district continues to have in authorising facility payments.
Greater transparency around the allocation of basket funds has improved providers attitudes towards district managers and reduced conflict within the district; however, some district managers were unhappy about their loss of power, and there were constraints to visiting facilities in some areas. The implementation of HBF-DHFF was reported in one district to have changed the attitude of health workers towards the district-level managers: since they now know the actual amount of budget and funds they have, they have therefore started to make informed decisions to guide their planning and implementation. The introduction of accountants at the health center level has helped to increase revenues, which also helps them to address a number of the challenges to improve service provision. District level managers also identified increased transparency as contributing to fewer conflicts between health facilities and the district level, as well as among district managers. One District Medical Officer noted:
“First it [RBF and HBF-DHFF] eliminated conflicts between the facilities and the DMO, and between the DMO and the director, because there is no place where the DMO gets into a dispute with the director on the misuse of funds allocated for purchasing medicines.”
However, other district level managers were more critical. Some of them indicated that they prefer “top-down” governance over facility self-authority, and several examples were mentioned in which district managers tried to overrule facility priorities. For example, some health facilities were advised to set aside part of their RBF bonus to procure laptops, although this investment was not a priority for the facilities. An observation by the research team also suggested that the district level managers in some cases interfere unnecessarily. In one case, an ultrasound machine broke, and the health workers did not have plans to fix it. However, the District Medical Officer ordered the repairs and for the repairs to be paid by the facility without prior agreement with the facility management.
5. Effects of RBF on community health worker performance
5.1 Research questions and key findings
RBF provides incentives for community health workers (CHWs) for conducting home visits, escorting pregnant women for delivery at health facilities, and for timely reporting on maternal and child deaths.
This chapters addresses the following research questions:
- How has RBF affected CHW performance?
- What factors have facilitated and inhibited change?
Key findings about the effect of RBF on CHW performance include:
- Community health workers report that RBF has significantly increased the number of women escorted for delivery.
- Many community health workers report that RBF increased the number of household visits. However, on average CHWs did not report a higher number of household visits in 2020 than they did in 2016.
- Many community health workers report that RBF increased their working hours and general availability. However, on average CHWs did not report more working hours in 2020 than they did in 2016.
- CHWs believed that the most important changes noted by community members because of RBF were that CHWs were more kind and patient, provided better education, and were more available to help.
Factors that facilitated change:
- Incentives to CHWs motivated them to make themselves more available, escort more women to delivery, and conduct more household visits.
- Training of CHWs improved their knowledge, motivation, and confidence.
- RBF incentives and reporting requirements created a mutual dependency between health facilities and CHWs which improved their cooperation and trust and facilitated higher utilisation of health services.
- Other programmes than RBF have also sensitised CHWs to visit households and encourage the use of health services.
Factors that inhibited change:
- Delays in RBF payments demotivated CHWs.
- Lack of report forms also prevented some CHWs from receiving their payments.
- Most CHWs report that lack of transport constrains their performance.
- CHWs sometimes get in each other’s way, creating a risk of a backlash from overwhelmed communities.
5.2 Community health worker performance
Community health workers report that RBF has increased the number of women escorted for delivery at health facilities. One CHW said,
“In the past, we didn’t have that thing, I mean, you spend your time escorting the mother to the facility, it wasn’t there, or insisting on her going to the facility, it wasn’t there. But after RBF, [it] came.” Another expanded and said, “The only thing changed is time for escorting a pregnant mother to give birth at health facility, because you are supposed to help her, twenty-four hours, to create a room of helping a mother during delivery. But that time, before RBF, we didn’t see the importance.”
Our survey data also shows that CHWs reported a significantly higher number of women escorted for delivery in 2020 compared to baseline in 2016.
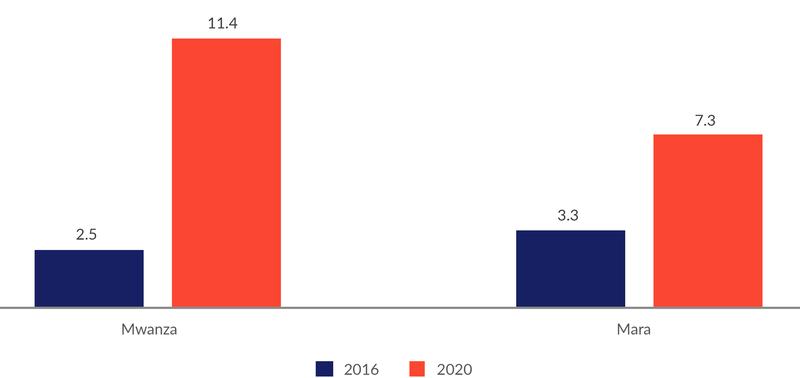
In Mwanza, the reported number of women escorted increased from 2.5 in 2016 to 11.4 in 2020. In Mara, the number went from 3.3 in 2016 to 7.3 in 2020. The increase was thus significantly higher in Mwanza than in Mara, suggesting that at least part of the increase is caused by RBF.
Many community health workers report that RBF increased the number of household visits. However, on average they did not report a higher number of household visits in 2020 than they did in 2016. One CHW said:
“In the past I used to visit few households but when RBF started to be implemented the number of households increased. In the past I used to visit even ten households. During the implementation of RBF, I visit twenty-four households.”
However, when comparing the number of reported household visits at baseline in 2016 and endline in 2020, it is less obvious that RBF has led to any increase in the number of visits. In fact, the CHWs report slightly fewer visits at endline compared to the baseline.
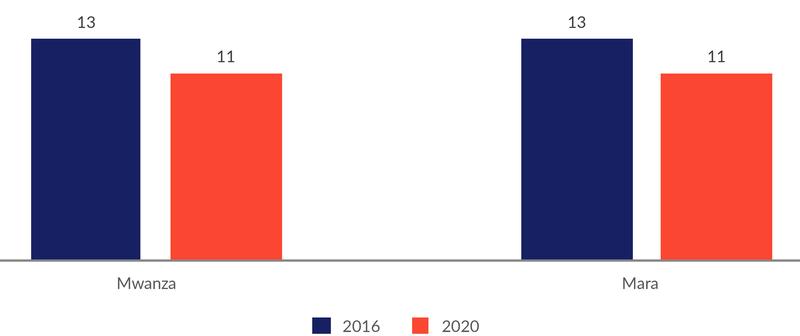
One CHW explained that a recent reduction in the number of household visits could be due to delayed payment,
“[Delay of payments] has damaged [CHW services] because, for example, the first time I was able to make visits to many homes expecting I will get something. But now I have found myself I don’t make visits to those homes I used to. For example, I could make up to 12 visits, but I only make 5.”
Another possible explanation is that the CHWs have saturated the communities, thereby decreasing the need for household visits. As one CHW said,
“The number of households which I visit now has decreased compared to the beginning because people have understood the meaning of going to the clinic early and delivering in the health facility… It has decreased because people are now aware.”
To explore whether the number of household visits had decreased due to the delay in RBF payments, we asked CHWs whether the number of household visits had increased or decreased during the past 1-2 years. However, contrary to our expectations, 70% of CHWs in both Mwanza and Mara reported an increase in the number of households visited during the previous 1-2 years (Figure 5.3).
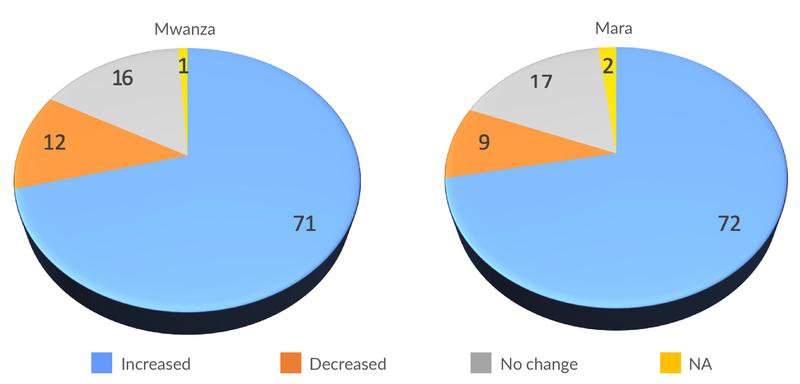
Hence, our data does not provide a clear answer to whether RBF caused an increase in the number of household visits or not. But apparently, most CHWs have a perception that they now are visiting more households.
Many community health workers report that RBF increased their working hours and general availability. However, on average they did not report more working hours in 2020 than they did in 2016. Several CHWs argued that RBF has made them make themselves more available:
“After (…) RBF, my working hours have increased. How? While at home and any time a patient can give me a call. Because after RBF training, we [left] our phone numbers to our patients. Therefore, someone may give a call around 23hours or 24hours, ‘I want to go to dispensary to deliver.’”
“ (…) now you can’t say [you] will work according to your timetable (…), now you can get a call while in shamba/cultivating and go. (…) previously there was no such issue.”
Others argued that the time serving each client had increased because they are more motivated to make sure that their messages are understood:
“The time has now increased. My responsibilities have increased. When people have an understanding of what you are doing you become motivated. If you were spending half an hour at least you will add one hour to make sure that what you are doing is understood by people.”
And some argued that they work more because they are motivated to visit more households:
“As of now, the working hours have increased. They have increased. Before I was working for four, or three hours, so we’re all scheduled the working time at the facility. But right now, for example, like visiting a household, you can plan to utilise four hours, but the task has not finished and what’s overwhelming is that maybe you meet with the cooperating clients, who leads you to another client or motivate you to move on to another household. And you find out you have spent even seven, eight, six hours. Yes, it’s not same as before.”
However, in the quantitative survey, the CHWs did not report a higher number of working hours per week in 2020 than they did in 2016 (Figure 5.4). While in Mwanza the number of working hours per week was 22 in both 2016 and 2020, the number declined from 27 to 22 in Mara. Again, we checked whether delays in payments during the past few years could have reduced work time in this period, but the responses here also point in the opposite direction: 65% of CHWs reported that hours worked had increased during the last 1-2 years, 25% reported no change, while only 8% reported a decline. In both regions, CHWs report that they now work 2-3 hours more per week than 1-2 years ago.

Hence, our data does not provide a clear answer to how RBF affected the working hours of CHWs.
CHWs believed that the most important changes noted by community members because of RBF was that CHWs were more kind and patient, provided better education, and were more available to help. We asked CHWs what they thought community members would say if they were asked about how RBF had changed the work of CHWs, thus making them reflect on the reality of change as others may have experienced it. There were three primary responses to the question:
CHWs have become more kind and patient; enjoyable to have involved in health matters. As one said, “[CHWs] have changed in behavior, how they attend the patient, very generously, well mannered, polite with compassionate.”
CHWs are providing better education. One CHW said; “They will tell you that there are changes in work performance; changes such as receiving education different from the way it was in the past.”
CHWs are more available; able to be reached frequently and at any time of day. One CHW said, “The community will appreciate me and they know all the services which I provide, I am a person who is committed regardless of the time.” Another said, “In the past, I used to come the health facility whenever I felt like it, on my own time, and the community and health facility were aware that I would visit a facility sometimes, but now all the time I am available at work.”
5.3 Factors that facilitated or inhibited change
Table 5.1 summarises factors that have facilitated and inhibited change in community health worker performance following the implementation of RBF. We distinguish between properties of the RBF scheme and contextual factors.

5.3.1 Facilitating factors
Incentives to CHWs motivated them to make themselves more available, escort more women to delivery, and conduct more household visits. CHWs reported greater motivation to work. Interestingly, the RBF bonus payments are referred to as “motivation,” thereby linking the idea of motivating CHWs with paying them. As one CHW said, “For example when you visit the pregnant woman, when you accompany her to the health facility there is some money which you are supposed to be paid, so we write a report at the end of the month, whenever you visit a mother you know that you will at least get something. So that is a motivation for me.” In this quote, the “motivation” could refer to either the payment or the desire to increase work; “motivation” appears to mean both. This increase in motivation is expressed in the rest of the changes as well.
Training of CHWs improved their knowledge, motivation, and confidence. A number of CHWs pointed to the role of RBF training in improving their knowledge, motivation, and confidence. One CHW said, “Education is important in motivation-- because it is difficult to discuss some things from your head without capacity building. You have to be given information on how things are. RBF did this for me.” Another said, “Before RBF, when you mention family planning its questions were very difficult to answer. But thanks to RBF and my supervisors at the facilities now, they have become very simple. When I explain to them, they get satisfied.” Yet another CHW added, “RBF has given us assurance that our activities are recognised by government.”
RBF incentives and reporting requirements created a stronger mutual dependency between health facilities and CHWs which improved their cooperation and trust and facilitated higher utilisation of health services. RBF incentives at health facility level made it more important for health workers to maintain a good working relationship with CHWs, because of CHWs’ role in bringing more patients to the facility.
“Yes, there are changes in one way or a certain percentage. To start with, there has been close relationship with facility health providers, meaning doctor and nurses; which seems that we now trust each other already. S/he receives my patient very quickly and provides services when I bring her here. So that shows the existence of a relationship and they are aware already about the importance of the community health worker in the facility.”
At the same time, improved quality of services at health facilities is valuable to CHWs because they can refer patients with increased confidence. Moreover, the requirement on CHWs to report their performance to the health facilities facilitated a closer relationship:
“At health facility, if you submit your reports at facility, means must work with health providers all the time, so there shall be close relationship. Also, you have to give knowledge to each other, such as how is this and what about there, when submitting reports which has created very close relationship, hence changes.”
Reported examples of improved cooperation include one health facility where health workers gave CHWs’ clients a higher priority, thereby rewarding both the CHWs and their clients for coming in escorted and together. In another area, health workers gave technical support to CHWs and improved their knowledge and authority with the clients.
In our CHW survey, 73% and 65% of CHWs in Mwanza and Mara claimed that they had received increased support from the health facility during the past four years (Figure 5.5).
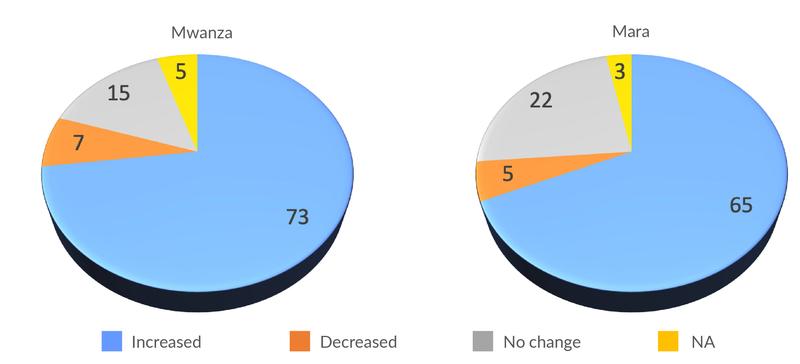
Importantly, closer cooperation and enhanced trust between health workers and community health workers is strengthening the bridge between communities and health facilities. It makes community members more confident that they will receive quality services if accompanied by a CHW.
“To be honest the community views us as a bridge that you cross because first they feel nice or they get comfort when they see us or when a person calls them to bring them to the clinic or to the escort her during delivery.”
“For example, my neighbour told me that she is preparing me so that I can accompany her. After two days she was in labour pain, she made a phone call to me. I was far away so she waited for me and I accompanied her. They believe that if you go with a community health worker [to the health facility] it creates trust. They will receive you well, but you will suffer if you go on your own, those are the changes which I have seen.”
Other programmes than RBF have also sensitised CHWs to visit households and encourage the use of health services. CHWs are important agents in many other programmes than RBF, e.g., nutrition programmes, maternal and child health programmes, and HIV/AIDS programmes. Household visits often play an important role in such programmes, and likewise the encouragements to use various services in the health system. Such contexts may be a fertile ground for the implementation of RBF incentives, increasing the likelihood of a positive response from the CHWs. On the other hand, if CHWs had already responded well to the sensitisation of the existing programmes, the scope for further improvements through RBF incentives may be more limited.
5.3.2 Inhibiting factors
Delays in RBF payments demotivated CHWs. As one CHW said, “Now our motivation has declined because it is better to tell someone that you are a volunteer and you won’t be paid anything so that one knows he is going to work but not expecting any payment, but if you convince someone that means you are doing something and you expect to get it and then you don’t get it, then you lose your motivation.” This has been a consistent and durable challenge, as our Nov. 2018 phone survey pointed to this as a top-three challenge in increasing RBF performance with 53% of the CHWs citing this.
Some noted that those CHWs who did not participate in RBF training tended to be more affected by delayed RBF payments, because of lower trust in the RBF scheme. As one CHW indicated, “Only two of us received RBF training, and after the training we came and gave the feedback to our fellow CHWs and gave them the forms. (…) We gave them the forms, but others have given up because of the money. But for us who received the training we will continue to fill the forms, but others have been affected by the funds, they are saying that we are lying to them because they haven’t received any money.”
Lack of report forms also prevented some CHWs from receiving their payments. In our November 2018 phone survey, 11% of CHWs signalled that the lack of available report forms was a challenge. This share appears to be higher now. One CHW said, “We started provision of services and implementation of the program but there were no reporting forms given to us. And at the end of a day they need reports which are directly written on those forms. So.. they didn’t bring forms, but we were told to write in forms and then they refused to accept some data. This may take us back and demoralise us.”
Most CHWs report that lack of transport constrains their performance. In the November 2018 phone survey, transport was the number one challenge to increasing RBF performance, with 70% citing this factor. Many CHWs discussed the challenges of doing household visits without reliable transportation. As one said, “That [area for household visits] is the end of the village, you struggle with the pregnant woman who is there, you have to walk. So we need to have some changes to enable us to work in an environment that motivates us to work. For example, the previous organisations were providing bicycles as a means of transport, a long time has passed so the bicycles are not working.” Without adequate transportation, it is difficult to increase household visits much. Furthermore, since other organisations have provided transport facilities, a sense of “fairness” may be violated if this issue is not addressed.
CHWs sometimes get in each other’s way, creating risk of a backlash from overwhelmed communities. Communities may become tired of very frequent visits by CHWs, for instance because of CHW duplication leading to one household’s receiving visits from multiple CHWs. “There will be a challenge because you may go to a certain area and be told that ‘we saw [another CHW] since a certain month,’ and still there are other CHWs.” Another said, “Sometimes when you visit them, they tell you ‘you visit us every day, you should also be giving us money, you are just talking’.” Another pointed out, “I have about two hundred and above households, and that is small area, and we are so many community health workers... Therefore, it will be a challenge because you may go to a certain area and be told that we saw him/her since a certain month (…).”
6. Effects of RBF on nutrition-related interventions
6.1 Research questions and key findings
This chapter addresses the following research questions:
- How has RBF affected the provision of nutrition services at health facilities?
- How has RBF affected the volume and quality of nutrition-related services by community health workers?
- What are the factors that have contributed or inhibited change in performance?
Key findings about RBF and the provision of nutrition services include:
- Stunting in children decreased significantly in Mwanza from 2014 to 2018.
- During this period, several nutrition-related programmes were implemented along with RBF. It is therefore not possible to isolate the effect of RBF on stunting.
- A large share of facility in-charges claimed that RBF has had a significant impact on nutrition services, but there are also some who claim there is little or no effect, especially in Mara where facilities have not yet received RBF funds.
- The change mentioned by most facility in-charges is an improvement in the content of care through more consistent provision of nutritional supplements and drugs. Some also mentioned that the number of patients has increased.
- RBF was perceived to reduce stock outs of nutritional supplements and drugs, both because of the additional resources and the incentives.
- Very few facilities in Mwanza had a stock out of nutrition-related drugs and equipment during our 2020 visit. Performance in Mara was not equally strong, but both regions saw improvements since 2016. Factors other than RBF have likely contributed, too.
- RBF incentives without sufficient resources to buy drugs can have perverse effects by causing reduced provision of nutrition services to avoid stock outs.
- RBF seems to have made CHWs bring more women and children to health facilities to receive nutrition services, especially through early ANC visits.
- There is considerable variation in what nutrition messages CHWs claim to provide. Most CHWs seem able to provide relevant and valuable counselling services, but many fewer seem to provide comprehensive and consistent advice.
- We do not know for sure whether RBF led CHWs to provide nutrition counselling to more women. There are several indications that it did, but there are also data that point in the opposite direction.
Key findings about factors that facilitated or inhibited change include:
- RBF programme features that facilitated change:
- RBF funds enabled health facilities to reduce stock outs of nutrition supplements
- RBF incentives induced health workers to maintain drugs in stock and to improve content of care during ANC consultation and consultations with children.
- Incentives for CHWs may have resulted in more household visits and more nutrition counselling.
- The combination of RBF at health facilities and incentives for CHWs increased cooperation and led to higher utilisation of services, especially earlier ANC consultations.
- RBF programme features that inhibited change:
- Delays in RBF payments reduced CHW motivation.
- Contextual factors that facilitated change
- CHW training in nutrition counselling through other programmes improved quality of nutrition messages.
- Contextual factors that inhibited change:
- Long distances and transport challenges for CHWs
- Poverty: nutrition advice may be difficult to follow
- Incomplete growth monitoring of children at health facilities
- Low awareness among health workers of the prevalence of chronic malnutrition (stunting)
6.2 The context
RBF aims to improve nutrition and child growth through (a) vitamin A supplementation for children between 12 and 59 months; (b) growth monitoring/promotion among children under five; and (c) home visits to provide nutrition/health education by community health workers (CHWs) during the first 1,000 days of life, from pregnancy to two years of age.
Stunting in children decreased significantly in Mwanza from 2014 to 2018. The Tanzania National Nutrition Survey 2018 showed that prevalence of stunting in children in Mwanza decreased significantly from 34.2% in 2014 to 26.2% in 2018. A smaller reduction was observed in Mara, but this change is not statistically significant. See Figure 6.1.
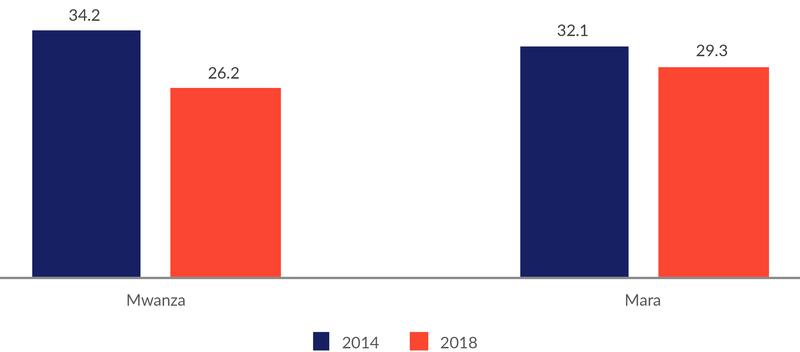
Source: Tanzania National Nutrition Survey 2018.
During this period, several nutrition-related programmes were implemented along with RBF. It is therefore not possible to isolate the effect of RBF on stunting. The most comprehensive programmes seem to have been implemented in Mwanza region. Most of the CHWs in our sample in Mwanza have been in touch with the Mtoto Mwerevu programme, implemented by IMA World Health. This programme offers CHWs a three-week training, as well as equipment for identification of acutely malnourished children. Other nutrition-related programmes include Boresha Afya (both regions), Kizaza Kipya (both regions) and Mama na Mtoto (Mwanza). These programmes seem to have been implemented in selected districts only.
The rest of this chapter sheds light on the likelihood of RBF contributing to these positive outcomes through its effect on the provision of nutrition services.
6.3 Nutrition services at health facilities
A large share of facility in-charges claimed that RBF has had a significant impact on nutrition services. One in-charge in Mara even said that this is “one of the most important components of RBF”. However, others hold a different view. One RBF coordinator in Mwanza claimed that “RBF’s impact on nutrition has been very minimal”, and a couple of facility in-charges in Mwanza reported that RBF has not affected the provision of nutritional supplements and drugs. Hence, there are probably strong differences across facilities in how RBF has affected nutrition services.
RBF increased health worker efforts to provide nutritional supplements and drugs to children and pregnant women. RBF thus improved the quality of service.
“Because we know that provision of iron, vitamin A, mebendazole are among the indicators which are required by RBF so that we can get paid … we try our level best to get those medicines and give to our clients.” (In-charge, Mara.)
Several respondents underscore the role of RBF indicators and performance incentives in enhancing motivation and effort:
“.. we have increased the effort after realising that this is an indicator that can also give you money in RBF.” (In-charge, Mara.)
While nutrition services clearly also were provided in the past, the effect of RBF has been to ensure that the services are provided more consistently:
“With RBF what we were implementing sluggishly will be implemented with speed without problems.” (DMO, Mara.)
RBF induced more patients to come to the facility for nutrition services. Some respondents also claim that RBF has increased the number of women and children that come to the clinic. This is seen as partly due to increased availability of drugs, but also because RBF makes CHWs visit more women and encourage them to visit the facility early for ANC visits:
“[There is an] increase in the number of people who comes to the facility due to the availability of vitamin A.” (In-charge, Mwanza.)
“RBF has come to contribute to a large extent along with the incentives given to community health workers [because] it encourages them to visit many women.” (In-charge, Mwanza.)
CHWs may also play a role in increasing the uptake of the services provided at the health facilities, as they teach pregnant mothers about the value of nutritional supplements:
“RBF has helped by using these community health workers. In the past when you give medicine to the mothers, they just keep it at home or throw it away, but nowadays they use them.” (In-charge, Mwanza.)
RBF reduced stock outs of nutritional supplements and drugs, both because of the resources and the incentives.
“Those [RBF] indicators have made us to make sure that those [drugs] are available, like vitamin A supplements and mebendazole….. We make sure that we have them all the time.” (In-charge Mwanza.)
The effect of RBF on stock out of nutritional supplements was noted mainly by respondents in Mwanza. Unlike health facilities in Mara, those in Mwanza have received RBF funds that have enabled them to buy drugs. This suggests that the resources that have been provided with RBF have played an important role in avoiding stock outs:
“…you may find that you are running out of nutrition items at your store or district, but with that money we can buy through local vendors.” (In-charge Mwanza.)
RBF performance incentives matter as well:
“If it is not there, it means there are marks that you will miss, so we make sure medicines are available all the time; mebendazole, folic, SP”. (In-charge, Mwanza.)
In Mara, there are also indications that RBF incentives have made some facilities increase their efforts to maintain drugs in stock, by obtaining from other facilities:
“But in the past, if they were out of stock, they would wait for MSD to bring it, but now if you see them are about to be out of stock, you even ask from the nearest facility.” (In charge, Mara.)
Others, however, maintained that little is going to change in Mara as a result of RBF until financial resources are provided:
“Before we receive the money we carry on with our normal routine.” (In charge, Mara.)
Very few facilities in Mwanza had a stock out of nutrition-related drugs and equipment during our 2020 visit. Both regions saw improvements since 2016., though performance in Mara was not as strong as that in Mwanza. Factors other than RBF have likely contributed, too. The positive development in Mwanza is shown in Figure 6.2.
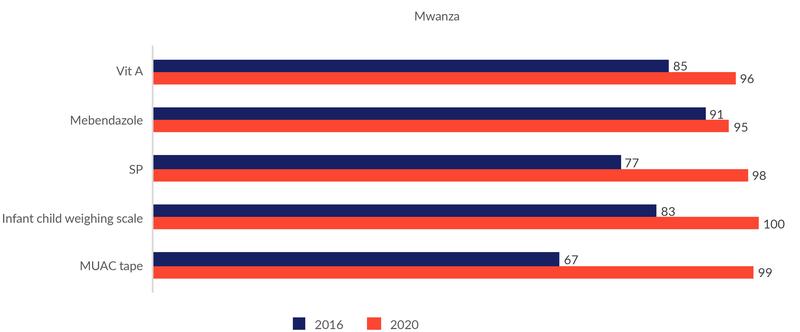
Figure 6.3 shows that facilities in Mara have also experienced a positive development in these indicators. However, if we can trust what facility in-charges in Mwanza report about the importance of RBF funds for reduced stock outs of drugs, the positive development in Mara can hardly be explained by RBF alone, as Mara had not yet received any RBF funds. Hence, other factors than RBF are most likely at play as well.
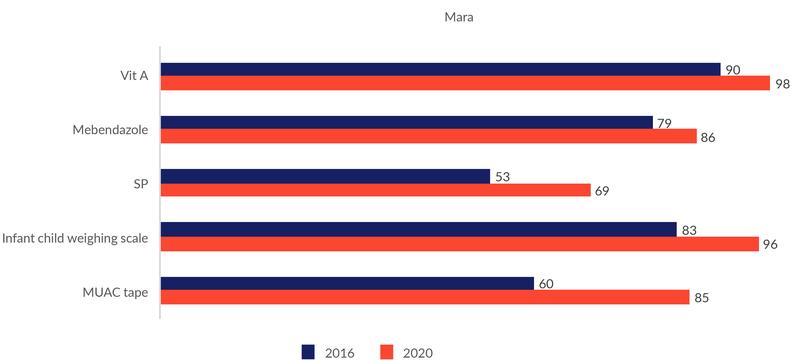
RBF incentives without sufficient resources to buy drugs can have perverse effects by causing reduced provision of nutrition services to avoid stock outs:
“Because every verification/assessment considers availability of those commodities, we economise to make sure all drugs/medicines are available”. (In charge, Mara.)
This underscores the importance of ensuring that the incentive for provision of drugs is stronger than the incentive to avoid stock outs.
6.4 Nutrition services through community health workers
CHWs provide preventive nutrition services by educating women about feeding practices for pregnant women and children. CHWs may also facilitate the provision of nutrition services at health facilities by encouraging women to attend ANC services or by identifying malnourished children and referring them for treatment at health clinics.
Whether or not RBF has contributed to improved nutrition services through CHWs depends on:
- Whether RBF made CHWs provide nutrition counselling to more women.
- What nutrition messages CHWs provide.
- Whether RBF made CHWs bring more women and children to health facilities to receive nutrition services.
We do not know whether RBF led CHWs to provide nutrition counselling to more women. First, we do not really know whether CHWs visited more households. Reports from CHWs themselves point in different directions. On the one hand, many CHWs claim that the number of household visits has increased. On the other hand, they report fewer household visits in 2020 than they did in 2016.
Second, even if RBF made CHWs do nutrition counselling in more households, the total number of women receiving nutrition counselling did not necessarily increase. The opposite may happen if RBF made CHWs move nutritional counselling from group settings, e.g., at the health facilities, and into people’s homes. CHWs indicated that this had indeed happened some places:
“.. the difference is that we were not visiting them in the villages, we were giving them education when they come here at the facility, not by following them to their homes. But after RBF we follow them to their households to educate them.” (CHW, Mwanza.)
It clearly takes more time to educate women in their homes than in larger groups, and it is not difficult to imagine that such a move may reduce the number of women reached, even though the number of household visits has increased. This is in fact not an unlikely outcome given the relatively modest increase in number of hours spent per week as a CHW. However, we do not know how common this pattern is. Other respondents claimed that RBF represented less of a change when it comes to nutrition counselling, as the Mtoto Mwerevu programmes also encouraged home visits.
“‘Mtoto Mwerevu’ was also pushing us to visit households. That is why I am saying it does not much differ.” (CHW, Mwanza.)
There is considerable variation in what nutrition messages CHWs claim to provide. Most CHW mention some key nutrition messages, but significantly fewer seem to provide comprehensive and consistent advice. A large share of the respondents said that they advise women to do exclusive breastfeeding for six months. Quite a few also mentioned continued breastfeeding until the child is two years old. Some also mentioned the importance of immediate breastfeeding after delivery (colostrum).
Pregnant women are advised to have a varied diet. Some also advise the pregnant woman to take nutritional supplements such as iron and iodine.
A few CHWs adopt a more systematic approach by teaching women about different categories of food and their properties:
“I explain to her for example the types of food for energy, food for immunity, food for body building and food for heat production, about five categories, so you instruct her to take food from those five categories.” (CHW, Mwanza.)
The patterns observed in our interviews are quite consistent with data collected from phone interviews with 105 CHWs in Mwanza in November 2018 (Table 6.1), where around 50-60% of CHWs claim to talk about exclusive breastfeeding, diet during pregnancy, diversity of diet for children, and frequency of feeding children, while other messages are provided by fewer CHWs.

Source: Binyaruka, Mæstad, and Somville (2019). RBF process evaluation. Results from phone survey #2.
Unfortunately, we do not have comparable phone survey data for the Mara region. Based on the qualitative interviews, however, CHWs in Mara appear to provide somewhat less comprehensive and less consistent nutrition messages than their fellows in Mwanza.
Such a difference might be explained by different levels of training. A higher share of CHWs have received training in nutrition counselling in Mwanza than in Mara during the past three years (83% in Mwanza vs 65% in Mara). See Figure 6.4.
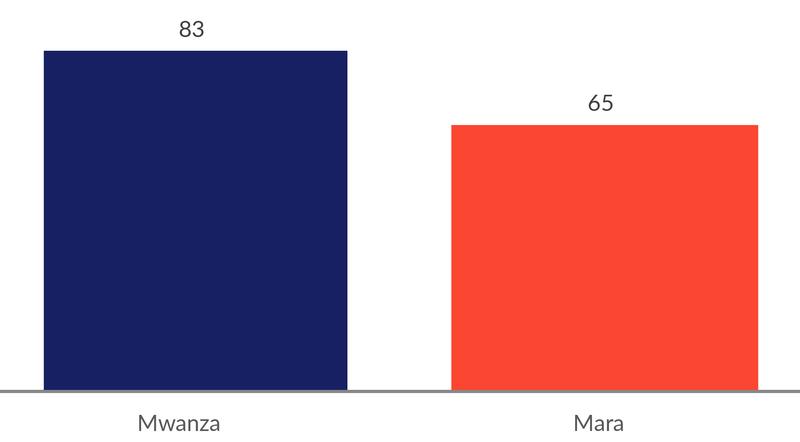
The quality of training may also differ. Quite a few CHWs in Mwanza appear to have attended a three-week training provided by the Mtoto Mwerevu project. This is a fairly extensive training in this context.
“Mtoto Mwerevu has contributed by increasing education on children under the age of five when it comes to nutrition. First, they have taught us all five groups of food, how to use the food and how to prevent diseases and how to care for a child or pregnant woman by reducing her workload, for example, giving her time to rest and scheduling time to eat when it comes to nutrition.” (CHW, Mwanza.)
RBF seems to have made CHWs bring more women and children to health facilities to receive nutrition services, especially through early ANC visits. In our 2018 phone surveys with CHWs in Mwanza, a majority of CHWs claimed to discuss antenatal services during home visits. Our qualitative interviews also leave a clear impression that CHWs consistently promote early visits to health clinics for ANC and other services.
“[I] educate the mothers that once they feel that they are pregnant they should start attending clinic so as to get quality services that will protect the unborn baby from problems.” (CHW, Mwanza.)
Several facts suggest that RBF may have played a role in promoting earlier ANC visits through CHWs. First, RBF may have resulted in more frequent home visits, where ANC services are one of the most frequently discussed topics:
“RBF has enabled us to visit households and talk; … a child to attend at clinic in time, … a pregnant woman to attend in time. We walk because the RBF target says so; just walk household to household and don’t stay idle.” (CHW, Mara.)
Second, due to incentives to escort women for delivery, CHWs are more eager to establish early contact with pregnant women and follow them throughout the pregnancy:
“You visit the mother who has a pregnancy that is three months old, you educate her until the time when she goes for delivery…, you visit her from time to time, … we were not doing that in the past.” (CHW, Mwanza.)
Finally, quality improvements of services at health facilities as a result of RBF seem to have made CHWs more eager to promote the use of their services. This relates to an overall strengthening of the relationship between households, CHWs, and the health facilities:
RBF seems to have created a stronger mutual dependency between CHWs and HWs at the facilities. (See Chapter 5). This mutual dependency creates a sense of cooperation: CHWs bring patients, and HWs provide quality care.
6.5 Factors that facilitated or inhibited change
Table 6.2 summarises key factors that have contributed to or inhibited effects of RBF on nutrition services.
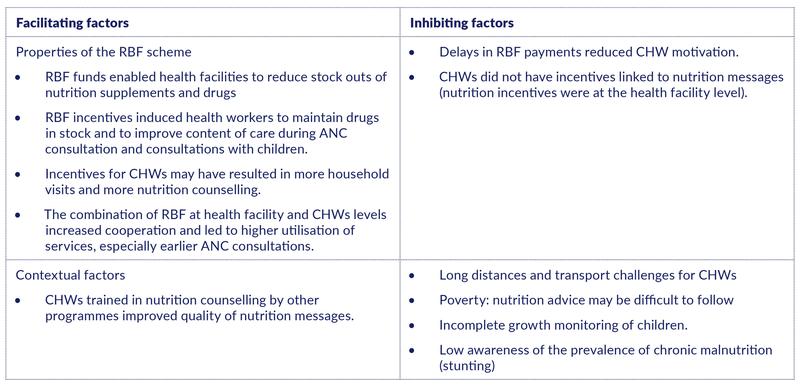
The factors that have facilitated change have been extensively discussed above. The following quotes further underscore the importance of the RBF incentives for the performance of CHWs:
“In the past we were not so much motivated to give education on nutrition but currently we have been motivated because of the system….The difference is that for example in the past I used to visit few households but when RBF started that is when I put more efforts.” (CHW, Mwanza.)
“I think that our work performance changed once we were aware that a person will be paid based on the work which he/she performed.” (CHW, Mwanza.)
Delays in RBF payments to CHWs is one of the factors that may have inhibited change:
“The payments have taken too long, like one year, so some people are not motivated to do the work.” (CHW, Mwanza.)
However, while these delays clearly make some CHWs frustrated, it is not possible to conclude from our data that it has caused a strong reduction in service provision. Some claim that the delays have had no effect on nutrition counselling:
“It hasn’t affected, because we continue to visit households and educate them”. (CHW, Mwanza.)
The fact that it has not been possible to directly incentivize nutrition messaging at the household level is probably also among the factors that inhibit RBF from further promoting nutrition services. While this issue was not mentioned by any of the respondents, it is a natural conclusion in light of the importance that health workers attach to incentives in explaining improvements in content of care.
Among the contextual factors that have been identified as impediments, the most frequently mentioned one is the issue of transport.
“… the thing which … causes challenges to us is the issue of transport. The hamlets are big like villages, and it is tiresome to us. The households are also far from each other. It becomes difficult for you to reach them, so you just find that you go to the nearby households.” (CHW, Mwanza.)
In our 2018 phone surveys, 70-80% of the CHWs mentioned transport as a constraint to further improve performance. On the other hand, some CHWs also mention that RBF funds have been a help in solving transport challenges:
“RBF has been able to solve minor challenges such as transport, so I have been able to reach households that are located far.” (CHW, Mwanza.)
Some CHWs also mention that household poverty is a constraint in ensuring uptake of nutritional advice.
“When you tell him/her maybe buy something, use this kind of food, maybe eat banana, eat fruits, eggs, s/he tells you; we don’t have money, please brings us money!” (CHW, Mwanza.)
In general, though, it appears that CHWs have been trained to adapt their advice to the economic conditions of the households and recommend food that is affordable, yet nutritious. People living in extreme poverty may nevertheless be unable to follow the advice.
Finally, results from our phone survey in February 2018 indicate that growth monitoring of children is incomplete. While almost all health workers say that they conduct growth monitoring, only 42% claim to measure children’s height.
We also observed low awareness among health workers of the prevalence of stunting. 79% of the health workers believed that the prevalence of stunting was in the range 0-10%, while the true figure was around 26% in Mwanza region, according to the Tanzania National Nutrition Survey, 2018. Our qualitative interviews with CHWs confirm that child malnutrition is not seen as a big issue:
“Now getting a child with malnutrition is very rare even on the streets where we go looking but finding a child with malnutrition I mean, maybe you can get one out of one hundred or two hundred children and still not severe malnutrition, probably a mild malnutrition.“ (CHW, Mwanza.)
While it is true that the prevalence of acute malnutrition is low (3.6% in Mwanza and 1.7% in Mara, according to the Tanzania National Nutrition Survey (2018)), it seems like the issue of chronic malnutrition is not receiving a lot of attention, neither among CHWs nor among health workers.
Acknowledgements
This work was funded by the World Bank and the Research Council of Norway (grant no. 234514).
The report was prepared by a team of researchers from Ifakara Health Institute (IHI), Tanzania; Chr. Michelsen Institute (CMI), Norway; and London School of Hygiene and Tropical Medicine (LSHTM), UK. We thank the administration of IHI for providing conducive research environment (i.e., field transport/vehicles, survey tool programming, data transfer and storage, recruitment of enumerators, training facilities, etc.) and the administration at CMI for its excellent support.
We sincerely appreciate all the guidance, facilitation, and time offered by the government officials from the Ministry of Health, Community Development, Gender, Elderly and Children (MOHCDGEC); the President’s Office of Regional Administration and Local Government (PORALG); and the Ministry of Finance and Planning (MOFP). We also acknowledge the extensive and valuable feedback provided by representatives from the Government of Tanzania and the World Bank, through comments to the report and feedback to presentations of the findings.
We also extend our acknowledgement to all respondents during data collection (i.e., health care workers, community health workers, members of the health facility governing committee, health managers at the district and regional level, and representatives from national level). We appreciate the facilitation in terms of granting permissions from PORALG and MOHCDGEC to ensure a smooth fieldwork for data collection in Mwanza and Mara regions.
Finally, we acknowledge the tremendous effort of the field research team (field coordinators, supervisors and enumerators) in ensuring a successful data collection process.
References
Government of Tanzania (2017). Direct Health Facility Financing. Presentation held 17.07.2017.
Ntuli A. Kapologwe, Albino Kalolo, Stephen M. Kibusi, Zainab Chaula, Anna Nswilla, Thomas Teuscher, Kyaw Aung, and Josephine Borghi (2019) Understanding the implementation of Direct Health Facility Financing and its effect on health system performance in Tanzania: A non-controlled before and after mixed method study protocol. Health Research Policy and Systems, 17.11.
Ministry of Health and Social Welfare (2015). Results-Based Financing. Design Document. August 2015.
Ministry of Health, Community Development, Gender, Elderly and Children and Presidents Office Regional and Local Government (2017). Decentralized Direct Facility Financing. Concept note and Roadmap. Draft, 15.02.2017.
Appendix 1: Theories of change
This appendix explains the pathways by which RBF and HBF-DHFF are intended to achieve their objectives, points out critical assumptions necessary for the schemes to work as intended, and identifies possible unintended effects.
A1.1 RBF
Pathways: RBF rests on four central components: 1) increased funding to health facilities, which enable them to increase the quantity and quality of services; 2) increased autonomy of management of funds, which may improve efficiency and motivation; 3) financial incentives to both health facilities and health workers, which may increase motivation and efforts to improve service availability, productivity, and the quality of care (the allocation mechanism of the staff bonus also provides incentives for reduced absenteeism); 4) data collection and verification, which may improve the available of quality data for improved decision making, improve supervision from the district level, and strengthen accountability mechanisms (and avoid misreporting).
Assumptions: Health workers are assumed to be motivated by financial rewards and/or by increased autonomy, and to have the possibility to engage in various activities that will improve quality indicators and attract more patients to the facility (such as improving the physical infrastructure, the availability of drugs and equipment, or simply being more pleasant to the patients, increasing outreach and opening hours, improving transportation, or reducing user costs).
Other critical assumptions are that RBF is implemented well enough to make health workers have trust in the scheme, that health workers understand the scheme and how to respond to the incentives, that the incentives are sufficiently strong to lead to change in behaviour, and that these changes will be appreciated by patients to the extent that they increase service utilisation.
Possible unintended effects: These include deterioration of non-incentivised (aspects of the) services, misreporting and corruption, and the use of non-ethical strategies to attract more patients. Another risk often emphasised in the literature is that of crowding out the workers’ intrinsic motivation, but the opposite is also possible.
More about how RBF is supposed to affect nutrition outcomes:
Objectives: RBF is meant to improve nutrition and child growth through (a) vitamin A supplementation for children between 12 and 59 months; (b) growth monitoring/promotion among children under five; and (c) home visits to provide nutrition/health education by community health workers (CHWs) during the first 1,000 days of life, from pregnancy to two years of age.
Pathways: The interventions are expected to contribute to improved nutrition through the following pathways: (a) vitamin A supplementation improves child growth by reducing the severity of infections; and (b) nutrition education and promotion at the facility level and the community level (including promotion of adequate infant and young child feeding and care and maternal nutrition care) helps children grow better during the first 1,000 days of life.
Assumptions: RBF will induce health workers to make efforts to improve vitamin A supplementation and perform growth monitoring more systematically. Health workers are able to ensure adequate supplies of drugs and equipment for this to happen. Health workers and community health workers will provide nutrition education where needed. RBF to community health workers based on the number of home visits will induce community health workers to make more visits. Community health workers have sufficient knowledge to provide adequate nutrition counselling, and they are willing to spend time on this task.
A1.2 HBF-DHFF
Pathways: The key elements of the HBF-DHFF programme are 1) increased autonomy in planning, budgeting and spending, which is assumed to increase engagement of facility staff and health facility governing committees, drawing on their knowledge of the local context, and thereby improve efficiency and the quality of services; 2) financial incentives for health facilities, as they may increase their resources by having more OPD consultations.
Assumptions: Health workers and facility governing committees are motivated by increased autonomy and/or by performance incentives for the facility, to the extent that they want to take action to improve service delivery. Health workers have the necessary resources and opportunities to implement the actions that will improve service delivery. These actions will be sufficient to increase the quality and/or utilisation of services.
Furthermore, for the HBF-DHFF to be successfully implemented, providers must understand how they can obtain (more) funds and how they can plan and spend resources to improve efficiency, which requires necessary knowledge about the PlanRep tool and the FFARS system. The supporting infrastructure for these systems needs to be in place, including necessary support from the district level. All facilities need staff that can support financial management and generate financial reports, either in-house staff or assistance from the health centre level. Health facility governing committees must be in place to provide oversight of the use of funds.
Possible unintended effects: As HBF-DHFF involves funds surpassing the district level, HBF-DHFF may be perceived as a threat by district managers, limiting their control and influence of resource allocation. This might harm the relations between facilities and district managers and result in reduced support and supervision to facilities.
Other possible unintended effects include: deterioration of services and quality aspects that will not affect the number of OPD consultations, misreporting performance indicators, use of non-ethical strategies to attract more OPD patients, reduced trust between communities and providers resulting from weak planning and financial management, and corruption.
Appendix 2: Estimated effects of RBF
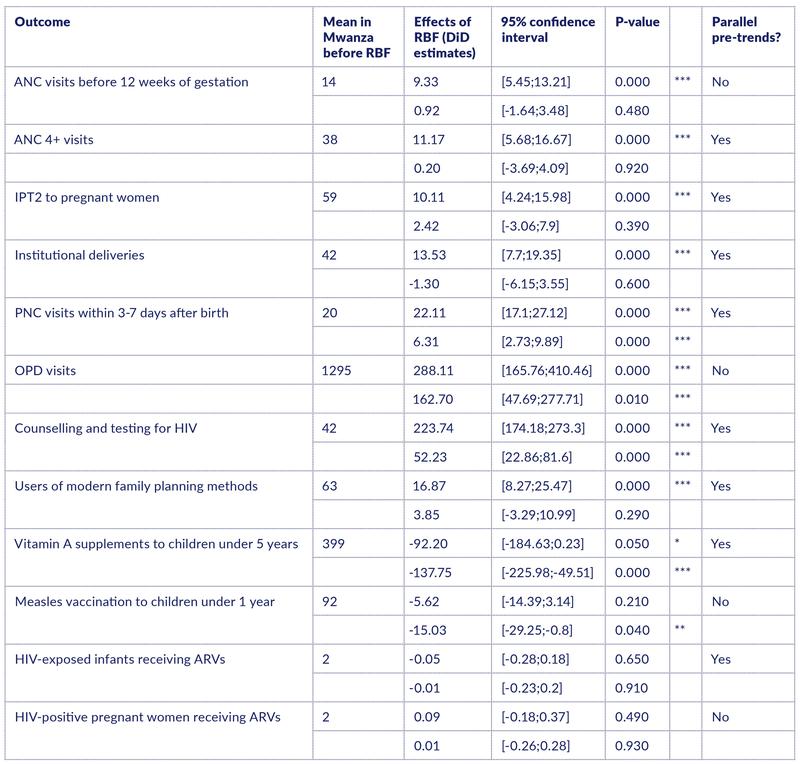
Note: The means before RBF in Mwanza are calculated based on data from 2015 and the first quarter of 2016. For each outcome, the first DID estimate is calculated before RBF starts in Mara and the second estimate before HBF-DHFF starts in both regions. The estimations include facility fixed effects and time (quarter) fixed effects. The standard errors are clustered at the facility level. Stars indicate a p-value; ***<0.01, **<0.05 and *<0.1. “Yes” in the column “Parallel pre-trends?” means that the test of non-parallel trends was rejected.